In de novo heart failure with reduced ejection fraction (HFrEF) current guidelines support, an initial double combination therapy with angiotensin converting enzyme inhibitors/angiotensin-receptor blockers and betablockers, only adding minerocorticoid receptor antagonists if after treatment optimization left ventricular ejection fraction (LVEF) is still under 40%. An initial triple combination therapy could be an attractive initial approach in the stability phase after an acute HF episode in debut HFrEF; which is what we describe in this report and analyze the factors related to the treatment with triple neurohormonal blockade (TNHB).
MethodsRetrospective study of patients discharged from our centre between January 2009 and January 2016 with de novo HFrEF after an acute HF episode with these criteria: 15–85 year-old, creatinine ≤2.5mg/dL, potassium <5.5mEq/L and no organic severe valvular disease.
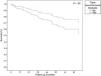
ResultsA total of 280 patients fulfilled the criteria, 58% of them were discharged on TNHB. Mean age was 65.4±12.5 years, LVEF 29.8±7.3% and median NT-ProBNP 2917pg/mL. After a mean follow-up of 43.4±26.6 months, 72 patients died (25.7%), with a mean survival of 76 months. Patients treated with TNHB had a better risk profile (they were younger, better creatinine and lower pulmonary pressures) but poorer LVEF (28.7±7.4% vs. 31.4±6.7%; P=.002). Mean survival on TNHB was better (months, 82.1±3.0 vs. 68.6±3.8; P=.007). Multivariate analysis showed that TNHB was an independent predictor of better survival (HR, 1.79; 1.05–3.05; P=.03).
ConclusionsTNHB is commonly used in debut HFrEF, especially in younger patients with worse LVEF. In our cohort TNHB was an independent factor related to better survival.
En la insuficiencia cardiaca con fracción de eyección reducida (IC-FEr) de novo las guías clínicas recomiendan el tratamiento combinado doble de inhibidor de la enzima de conversión de angiotensina/bloqueadores de receptores de angiotensina II y bloqueadores beta, añadiendo antagonistas de aldosterona solo si tras el tratamiento optimizado la fracción de eyección del ventrículo izquierdo (FEVI) es inferior al 40%. El tratamiento tripe combinado inicial podría ser atractivo en pacientes con IC-FEr de novo, lo cual se describe en este trabajo y se analizan los factores relacionados con el triple bloqueo neurohormonal (TBNH).
MétodosEstudio retrospectivo de pacientes dados de alta de nuestro centro entre enero de 2009 y enero de 2016 con IC-FEr de novo con estos criterios: edad: 15-85 años, creatinina: ≤2,5mg/dl, potasio: <5,5mEq/l y sin valvulopatía orgánica grave.
ResultadosSe analizó a 280 pacientes, se dio de alta con TBNH al 58%. La media de edad fue de 65,4±12,5 años, FEVI 29,8±7,3% y mediana de NT-ProBNP 2917pg/ml. Tras un seguimiento medio de 43,4±26,6 meses, 72 pacientes fallecieron (25,7%), con una supervivencia media de 76 meses. Los pacientes tratados con TBNH presentaban un perfil de riesgo menor (más jóvenes, con mejor creatinina y presiones pulmonares menores), pero peor FEVI (28,7±7,4% frente a 31,4±6,7%; p=0,002). La supervivencia media con TBNH fue mejor (meses: 82,1±3,0 frente a 68,6±3,8; p=0,007). El análisis multivariado mostró que el TBNH fue un predictor independiente de mejor supervivencia (HR= 1,79; 1,05-3,05; p=0,03).
ConclusionesEl TBNH se usa frecuentemente en la IC-FEr de inicio, especialmente en pacientes más jóvenes y con peor FEVI. En nuestra cohorte además, se asoció independientemente a mayor supervivencia.
Heart failure with reduced ejection fraction (HFrEF) is related to bad prognosis at midterm1: 3 drug classes – betablockers, angiotensin converting enzyme inhibitors (ACE-i), or angiotensin receptor blockers (ARB) and mineralcorticoid receptor antagonists (MRA) – and recently, angiotensin receptor neprilysin inhibitors (ARNI), have demonstrated to improve survival and quality of life in this condition.2–6
Current European guidelines recommend starting betablockers and ACE-i/ARB together in debut HFrEF, although there are no prospective trials evaluating this strategy versus the sequential initiation of drugs. Adding MRA is recommended if after dose optimization the patients is symptomatic and left ventricular ejection fraction (LVEF) is still ≤35%,2 which in the real-world setting takes several months. European guidelines also recommend starting the neurohormonal blockade during hospitalization in the stability phase after an acute heart failure episode. This recommendation is based in a relatively weak evidence.7,8 More recently, the TRANSITION and PIOONER-HF trials have demonstrated that starting ARNI in this scenario is safe and improves heart failure parameters, even in debut heart failure patients.9,10
A recent update of the Canadian Society of Cardiology heart failure guidelines, support the initial triple neurohormonal blockade (TNHB) with betablockers, ACE-i/ARB and MRA in debut HFrEF11 in opposition to the sequential strategy of the European and American heart failure guidelines. This recommendation is not based in any study, but, despite controversial, might represent a not uncommon real life approach. Initial TNHB could be seen as an attractive idea as theoretically allows more renin-angiotensin-aldosterone system blockade from the diagnosis, which might allow an earlier and stronger modification of the course of the disease, with the side effects of MRA as the “yang” of this strategy.
In this paper we perform an exploratory analysis of the frequency and the prognostic impact of TNHB in a cohort of patients discharged from our centre with new onset HFrEF. This is, to the best of our knowledge, the first time this kind of analysis is reported in the literature.
MethodsStudy populationSingle-centre retrospective cohort study of patients discharged from the cardiology department of the Hospital Alvaro Cunqueiro (Vigo, Spain) between January 2009 and January 2016 with the diagnosis of new onset HFrEF (pre-discharge LVEF ≤40%). Additional inclusion criteria were: age 15–85 years, creatinine ≤2.5mg/dL, potassium <5.5mEq/L and no severe primary valvular disease (the absence of significant aortic stenosis or regurgitation, mitral stenosis, tricuspid stenosis or mitral or tricuspid regurgitation of other aetiology apart of functional). The objective of these criteria was to select a population with dilated cardiomyopathy and left ventricular dysfunction related to ischaemic heart disease without general contraindications for ACE-i/ARB or MRA.
DefinitionsNew onset heart failure was defined as the first episode of heart failure leading to the diagnosis of the condition. HFrEF was defined according to 2016 ESC heart failure guidelines.2 Primary valvular disease was defined as per 2017 ESC valvular heart disease guidelines12; it was considered significant when the valvular disease could meaningfully contribute to the development of heart failure: severe aortic stenosis or regurgitation, severe mitral stenosis or regurgitation, severe pulmonary stenosis or regurgitation or severe tricuspid stenosis or regurgitation. Chronic renal failure was defined as baseline creatinine ≥1.5mg/dL. TNHB was defined as the treatment at discharge with betablockers, ACE-i/ARB and MRA. The non-TNHB group included those patients not treated with TNHB (Fig. 1).
Follow-upData were collected in an anonymous database and analyzed after the approval of the local ethical committee. Patients were followed up as per local hospital protocols and under their clinician judgement. Patients were discharged and drug titration was performed following heart failure guidelines. Follow-up events were updated up to April 2018.
Statistical analysisResults were expressed as mean plus standard deviation or percentages, the most appropriate for each variable. Statistical differences were analyzed with Student t-test or chi-square as appropriate. Survival analysis was performed with the Kaplan–Meier curves and long-rank test was used to evaluate statistical significance. Variables consistently related in the literature to worsen prognosis in HFrEF entered a multivariate Cox regression survival model to evaluate statistical significance. The discriminative accuracy of the model was evaluated using the area under the ROC curve (c-index). Results were expressed as hazard ratio (HR) with 95% confidence interval (95%CI). A P value <.05 was considered significant. All analyses were performed using SPSS 19.0 (SPSS Inc, Chicago, IL, USA).
ResultsFrom 665 patients with debut HF, 317 had HFrEF. A total of 37 were excluded of the analysis for not meeting the additional inclusion criteria. Finally, 280 discharged patients fulfilled the study criteria. Of them, 162 (57.9%) were discharged on TNHB. The remaining 118 patients (42.1%, the non-TNHB group) were discharged on any combination of betablockers and ACE-i/ARB, betablockers and MRA or ACE-I/ARB and MRA (83 patients, 29.6% of the whole cohort and 70% of the non-TNHB group) or on just one heart failure drug (35 patients, 12.5% of the whole cohort and 30% of the non-TNHB group) (Fig. 1). In general, 85.4% of the patients were discharged on betablockers, 85.7% on ACE-i or ARB, 70% on MRA, 77.1% on furosemide, 53.9% on statins and 8.6% on ivabradine.
Baseline characteristics of the whole cohort and stratified depending on TNHB are shown in Table 1; 36.8% of patients had ischaemic heart disease as the cause of left ventricular dysfunction; 63.2% of patients had a dilated cardiomyopathy of different aetiologies. Mean age was 65.4±12.5 years, mean LVEF was 29.8±7.3% and tricuspid annular plane systolic excursion was 16.8±4.4mm. Discharge creatinine was 1.14±0.3mg/dL, discharge serum potassium was 4.2±0.6mEq/L and median N-terminal prohormone of brain natriuretic peptide (NT-ProBNP) at admission 2917pg/mL. After a mean follow-up of 43.4±26.6 months, 72 patients died (25.7% of the cohort), with a mean survival of 76.1 months (Table 2).
Baseline characteristics of the whole cohort and analyzed according to different treatment strategies.
| Full cohort (280) | No TNHB (118) | TNHB (162) | No TNHB vs. TNHB P | |
|---|---|---|---|---|
| Age | 65.5 (12.5) | 69 (11.4) | 62.9 (12.7) | <.01 |
| Age >70 years | 41.1 | 51.7 | 33.3 | <.01 |
| Weight (kg) | 78.99 (12.29) | 78.56 (15.48) | 79.28 (16.87) | .73 |
| Male gender | 73.6 | 75.4 | 72.2 | .55 |
| Current smoker | 21.8 | 14.4 | 27.2 | .03 |
| Hypertension | 53.2 | 59.3 | 48.8 | .08 |
| Dyslipidemia | 48.6 | 55.1 | 43.8 | .06 |
| Diabetes Mellitus | 27.9 | 32.2 | 24.7 | .16 |
| Previous myocardial infarction | 16.8 | 23.7 | 11.7 | <.01 |
| Atrial fibrillation | 24.6 | 29.7 | 21 | .23 |
| Valvular prosthesis | 3.9 | 5.1 | 3.1 | .39 |
| Previous stroke | 7.5 | 11 | 4.9 | .06 |
| Chronic renal failure | 9.3 | 12.7 | 6.8 | .12 |
| COPD | 13.6 | 16.9 | 11.1 | .16 |
| Aetiology | ||||
| Dilated cardiomyopathy | 63.2 | 55.9 | 68.5 | .03 |
| Ischaemic heart disease | 36.8 | 44.1 | 31.5 | |
| LVEF (%) | 30 (7.3) | 31 (7) | 28.7 (7.4) | <.01 |
| TAPSE (mm) | 17 (4) | 17 (5) | 17 (4) | .75 |
| RVESP (mmHg) | 46 (12) | 49 (15) | 43 (9) | .02 |
| Haemoglobin (g/dL) | 14 (7) | 14 (10) | 14 (2) | .69 |
| Creatinine (mg/dL) | 1.13 (0.3) | 1.20 (0.4) | 1.08 (0.3) | <.01 |
| Sodium (mEq/L) | 139 (3) | 139 (3) | 138 (3) | .37 |
| Potassium (mEq/L) | 4.2 (0.6) | 4.3 (0.6) | 4.2 (0.6) | .08 |
| NT-proBNP (pg/mL; median, p 25–75) | 2917 (1341–5548) | 2633 (1227–5579) | 3166 (1353–5507) | .20 |
| Total cholesterol (mg/dL) | 162 (39) | 159 (40) | 164 (39) | .26 |
| Uric acid (mg/dL) | 7.8 (2.2) | 7.8 (2.2) | 7.8 (2.2) | .97 |
| Albumin (mg/dL) | 3.7 (0.5) | 3.7 (0.5) | 3.7 (0.4) | .87 |
| TSH (UI/L) | 2.2 (2.3) | 2.2 (1.9) | 2.2 (2.4) | .92 |
COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal-pro-brain natriuretic peptide; TAPSE, tricuspid annular plane systolic excursion; TNHB, triple neurohormonal blockade; TSH, thyroid stimulating hormone; RVESP, right ventricular end-systolic pressure.
Unless otherwise specified, data are expressed as no. (%), mean (±) standard deviation or median.
Survival analysis. Univariate analysis.
| Alive (208) | Death (72) | P value | |
|---|---|---|---|
| Age | 63.4 (12.1) | 71.4 (11.9) | <. 01 |
| Age >70 years | 32.7 | 65.3 | <.01 |
| Weight (kg) | 80.4 (16.8) | 74.5 (13.5) | <.01 |
| Male sex | 74 | 72.2 | .76 |
| Current smoker | 21.6 | 22.2 | .98 |
| Hypertension | 51.4 | 58.3 | .33 |
| Dyslipidaemia | 49.5 | 45.8 | .59 |
| Diabetes Mellitus | 25.5 | 34.7 | .13 |
| Previous myocardial infarction | 15.9 | 19.4 | .48 |
| Atrial Fibrillation | 25.5 | 22.3 | .75 |
| Valvular prosthesis | 3.4 | 5.6 | .41 |
| Previous stroke | 4.8 | 15.3 | <.01 |
| Chronic renal failure | 7.2 | 15.3 | .11 |
| COPD | 10.6 | 22.2 | .01 |
| Aetiology | |||
| Dilated cardiomyopathy | 64.4 | 59.7 | .48 |
| Ischaemic heart disease | 35.6 | 40.3 | |
| LVEF (%) | 29 (7) | 31 (6) | .19 |
| TAPSE (mm) | 17 (4) | 16 (4) | .67 |
| RVESP (mmHg) | 45 (10) | 48 (16) | .23 |
| Haemoglobin (gr/dL) | 14 (2) | 15 (3) | .43 |
| Creatinine (mg/dL) | 1.12 (0.3) | 1.17 (0.3) | .24 |
| Sodium (mEq/L) | 138 (3) | 138 (4) | .51 |
| Potassium (mEq/L) | 4.2 (0.6) | 4.4 (0.7) | .03 |
| NT-proBNP (pg/mL; median, p 25–75) | 2913 (1097–5529) | 3281 (1869–5579) | .33 |
| Total cholesterol (mg/dL) | 165 (38) | 154 (43) | .03 |
| Uric acid (mg/dL) | 7.8 (2.2) | 7.9 (2.1) | .71 |
| Albumin (mg/dL) | 3.7 (0.5) | 3.6 (0.5) | .15 |
| TSH (UI/L) | 2.1 (1.8) | 2.4 (3.2) | .50 |
| Discharge treatment | |||
| TNHB | 63.5 | 41.7 | <.01 |
| Non-TNHB | 36.5 | 58.3 | <.01 |
| Furosemide | 75 | 83.3 | .14 |
| Statin | 56.3 | 47.2 | .18 |
| Ivabradine | 8.7 | 8.3 | .93 |
COPD, chronic obstructive pulmonary disease; COPD, chronic obstructive pulmonary disease; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal-pro brain natriuretic peptide; TAPSE, tricuspid annular plane systolic excursion; TNHB, Triple neurohormonal blockade; TSH, thyroid stimulating hormone; RVESP, right ventricular end-systolic pressure.
Unless otherwise specified, data are expressed as no. (%), mean (±) standard deviation or median.
TNHB group had some significant baseline differences compared to non-TNHB group. TNHB group had less ischaemic heart disease (31.5% vs. 44.1%; P=.03), was younger (62.9±12.7 vs. 69.0±11.4; P=.0001), more frequently smoker (27.2% vs. 14.4%; P=.03), with poorer LVEF (28.7±7.4% vs. 31.4±6.7%; P=.002) but better creatinine (1.08±0.3 vs. 1.21±0.4md/dL; P=.02) and lower estimated pulmonary pressures (43.26±9.38 vs. 48.85±14.61; P=.02). Mean survival on TNHB was better (months, 82.1±3.0 vs. 68.6±3.8; P=.007).
Age > 70 years, diabetes mellitus, previous stroke, weight, heart failure aetiology, TNHB and discharge creatinine were entered in a Cox regression survival model. The discriminative accuracy of the model evaluated by the area under the ROC curve was 0.75 (95% confidence interval [95%CI], 0.68–0.82). In this multivariate analysis, TNHB was still an independent predictor of better survival (HR, 1.79; 95%CI, 1.05–3.05; P=.03) (Fig. 2), meanwhile age > 70 years (HR, 0.39; 95%CI, 0.21–0.72; P=.003), previous stroke (HR 0.39; 95%CI, 0.18–0.84; P=.01) and weight (HR, 0.98; 95%CI, 0.96–0.99; P=.04) were independent predictors of worse survival.
To investigate factors independently related to TNHB prescription, previous myocardial infarction, heart failure aetiology, discharge creatinine, age, potassium, LVEF, right ventricular end-systolic pressure and hypertension were entered in a logistic regression model. Increasing age was the only factor independently related to less TNHB prescription (HR, 0.92; 95%CI, 0.88–0.97; P=.002).
DiscussionIn this retrospective analysis of a single centre cohort of patients with new onset HFrEF requiring hospital admission and that were successfully discharged, we show that treating patients from the diagnosis with THNB is related to better survival, even after adjusting for possible confounders. This is, to the best of our knowledge, the first time that the outcomes and frequency of TNHB as the initial strategy for debut HFrEF has been studied in the literature.
It is also of note that more than 50% of the patients of our cohort were discharged on TNHB, which probably resembles clinical practice in some European centres despite anticipating the current guideline algorithm, although there is no information in the literature. In our cohort, TNHB was less used mainly in elderly patients despite not having contraindication for MRA prescription, which it is in consonance with previously published works.13 TNHB in our cohort was mainly reserved to younger patients but with lower LVEF, thus clinician perception of disease severity was probably higher because of the LVEF, although, in fact, those not treated with TNHB had a more unfavourable clinical profile (worse renal function, higher pulmonary pressures and older age).
Anti-remodelling and anti-fibrotic effects of MRA have been related to improved clinical endpoints in the HFrEF pivotal trials.5,8,14 It is probable that these effects are taken into consideration when thinking about initial TNHB, added to betablockers and ACE-i/ARB, especially taking into account that in some MRA trials8 survival curves separate from the study beginning. Nevertheless, this practise has not been included in the latest ESC guidelines. Furthermore, it is also probable that MRA are added to patients with persistent congestion to increase the effect of loop diuretics, especially if coexists with hypokalaemia, instead of other diuretics and potassium supplements.
Current guidelines recommend initial dual neurohormonal blockade with betablockers and ACE-i/ARB although this strategy has not been proven in randomized prospective trials; thus prospective evidence of dual and triple neurohormonal blockade as the initial approach of patients with debut HFrEF could be considered at the same level. To this respect, it is considered that the potential benefit of initial dual neurohormonal blockade is related to the additional benefit of one drug over the other, after the results of the pivotal clinical trials, a rationale that might be correct in the same way adding MRA to this equation. The guidelines greatly encourage drug titration and algorithm-based new drug initiation during the follow-up in the heart failure or general cardiology clinics, but despite of this hospital discharge treatment is mainly unchanged in a great proportion of patients,15,16 which could also be involved in the benefit observed in our study with initial TNHB. It has been shown that a significant proportion of patients candidates to MRA do not receive the treatment, maybe because of therapeutic inertia.13 This is probably even truer in functional class II patients, as they are usually seen as “clinically stable”, but paradoxically get more benefit of drug optimization as it is probably easier to modify the HF progression from an earlier stage of the disease where ventricular remodelling is more probably reversible.6
MRA in HFrEF have demonstrated to improve the prognosis of HFrEF based on the results of 3 big trials: RALES, EPHESUS and EMPHASIS.5,8,14 The results of these trials have been translated into current 2016 ESC recommendations. Although also involving MRA, the rationale, design and objectives of other trials like ATHENA-HF17 are not really comparable with the results of the previous trials. The EPHESUS trial could also be considered considerably different to RALES and EMPHASIS as it was conducted only in patients with a recent acute coronary syndrome and only 15% had HF on the background, but in fact tested initial TNHB versus the standard treatment. In the EPHESUS trial more than 85% of patients were on ACE-i/ARB and 75% were on betablockers. Moreover, in the EPHESUS trial the benefit with eplerenone was only found in the group of patients already on betablockers and ACE-i/ARB. These pivotal MRA trials demonstrated a significant reduction of mortality on top of optimized betablockers and ACE-i/ARB in RALES5 and EMPHASIS.14 Whether this reflects the way clinical trials were conducted, waiting months on previous therapy to add a new drug that decreases mortality even more, with the evidence from trials in which survival curves separate from each other from the initial weeks on treatment and, taking into account that this rationale is not considered necessary when recommending adding betablockers to an ACE-i/ARB, might be the reasons why the Canadian update have recommended initial TNHB. Furthermore, recent results of the PIONEER-HF trial10 with sacubitril-valsartan come to challenge even more current recommendations, as it demonstrates, with more than 50% of naïve patients after an acute heart failure episode, further reductions of NT-ProBNP and HF hospitalizations compared to the standard therapy of ACE-i/ARB, which was also true in those with new onset HFrEF.
LimitationsThis is a retrospective study, so outcome data were not obtained at pre-specified times and treatment data were collected only at discharge, without information about drug withdrawal, initiation or dose titration during follow-up. However, it is well known that drug titration or drug initiation is poor after hospital discharge.15,16 This is a single-centre study, with potentially some unique characteristics related to discharge treatments and follow-up. The retrospective nature of this work makes it also susceptible to different bias. Discharge NT-ProBNP and discharge heart rate and blood pressure should ideally be entered in the multivariate analysis as they are strongly related to worse prognosis, but these were not available. Although re-hospitalization analysis would be desirable, these data was not available for analysis and with the data available we may not evaluate the influence of doses and its changes on survival risk. Although a propensity-score matching analysis would be an interesting addition to the Cox regression we show, the number of patients of our study does not make it useful.
ConclusionsIn debut HFrEF requiring hospital admission, being discharged on TNHB might be related to a better prognosis. This finding should be tested in prospective randomized placebo-controlled trials.
In de novo HFrEF, neurohormonal blockade with betablockers, ACE-i/ARB, ARNI and MRA improve the prognosis. The timing of drug introduction and optimization is not clear.
Does it contribute anything new?In de novo HFrEF, starting with triple neurohormonal blockade (betablockers, ACE-i/ARB and MRA) appears to be more effective than other kind of approaches.
None declared.