Anticoagulant therapy is one of the most widely used treatments for patients with atrial fibrillation, due to its ability to reduce mortality. However, anticoagulant therapy may cause potentially life-threatening complications. To alert clinicians to the side effects of anticoagulant therapy, which can be quite serious (major bleeding), identifying those risk factors that could justify a more conservative therapy approach, we present two cases of spontaneous hematoma occurring in women over age 75 years while undergoing anticoagulant therapy.
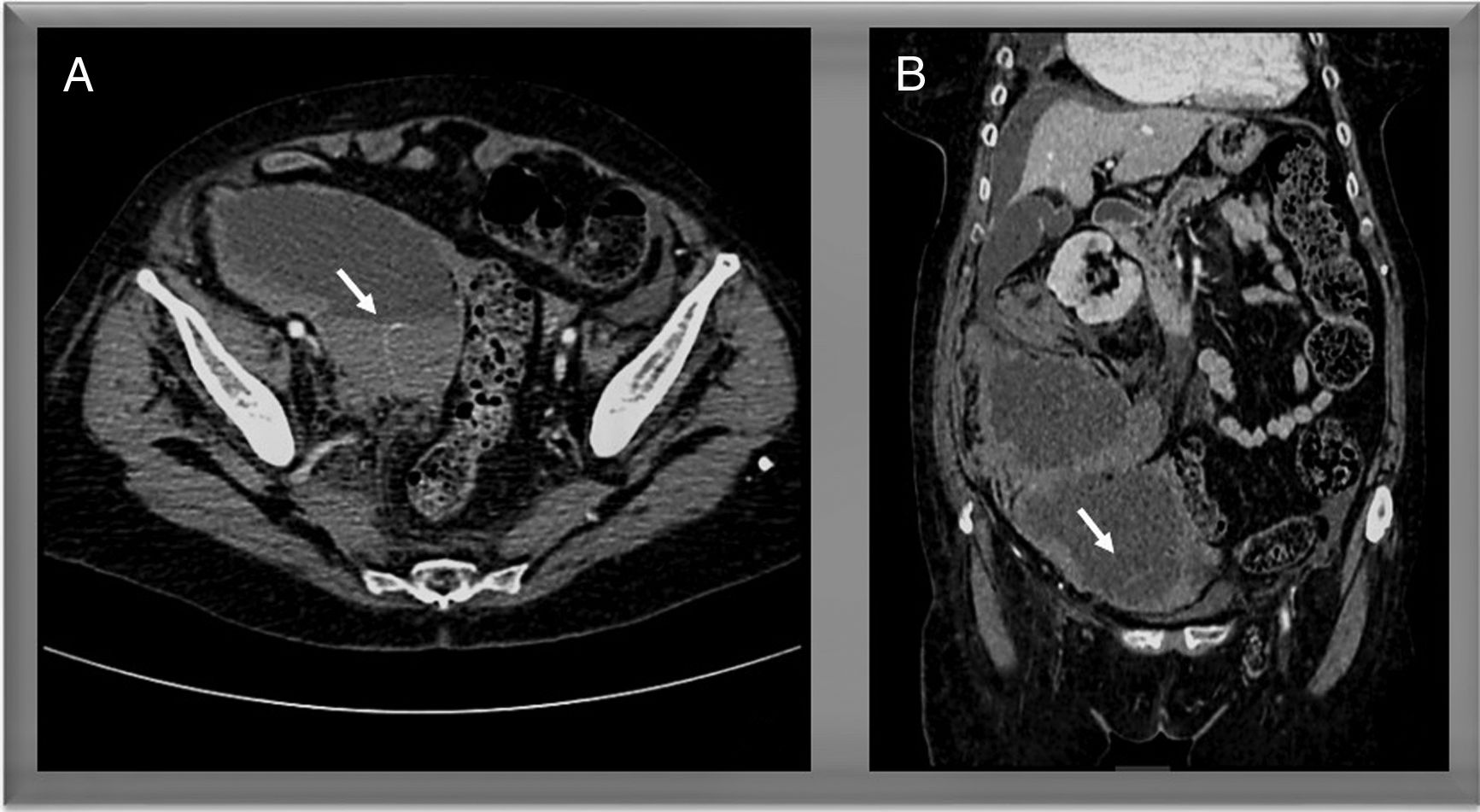
A 77-year-old female patient with a history of a mechanical mitral valve replacement and echocardiographic signs of severe pulmonary hypertension was admitted to our institution following a first episode of cardiac failure with signs of right cavity overload and moderate pleural effusion refractory to treatment with intravenous diuretics. A thoracentesis was ordered for drainage and laboratory testing. Before the procedure, the patient's usual treatment with warfarin was withheld and bridging treatment with low-molecular-weight heparin was started with enoxaparin at a dose of 60mg BID (the patient weighed 72kg, had a GFR of 44mL/min and INR of 1.7). On the second day after initiating treatment with heparin, the patient began to complain of diffuse abdominal pain, which later became localized in the right iliac fossa, showing signs of peritonism. Blood tests revealed severe anemia and lactic acidosis. The patient's hemodynamic condition deteriorated to progressive instability. An urgent computed tomography scan revealed a large retroperitoneal hematoma, with active bleeding in the right psoas muscle (Fig. 1). Hemodynamic support was provided with intravenous fluids, transfusion therapy, and vasopressors, and an emergency angiography was performed, failing to reveal active bleeding. During the procedure, the patient presented extreme bradycardia, with worsening consciousness and finally asystole. Cardiopulmonary resuscitation was provided, though unsuccessfully.
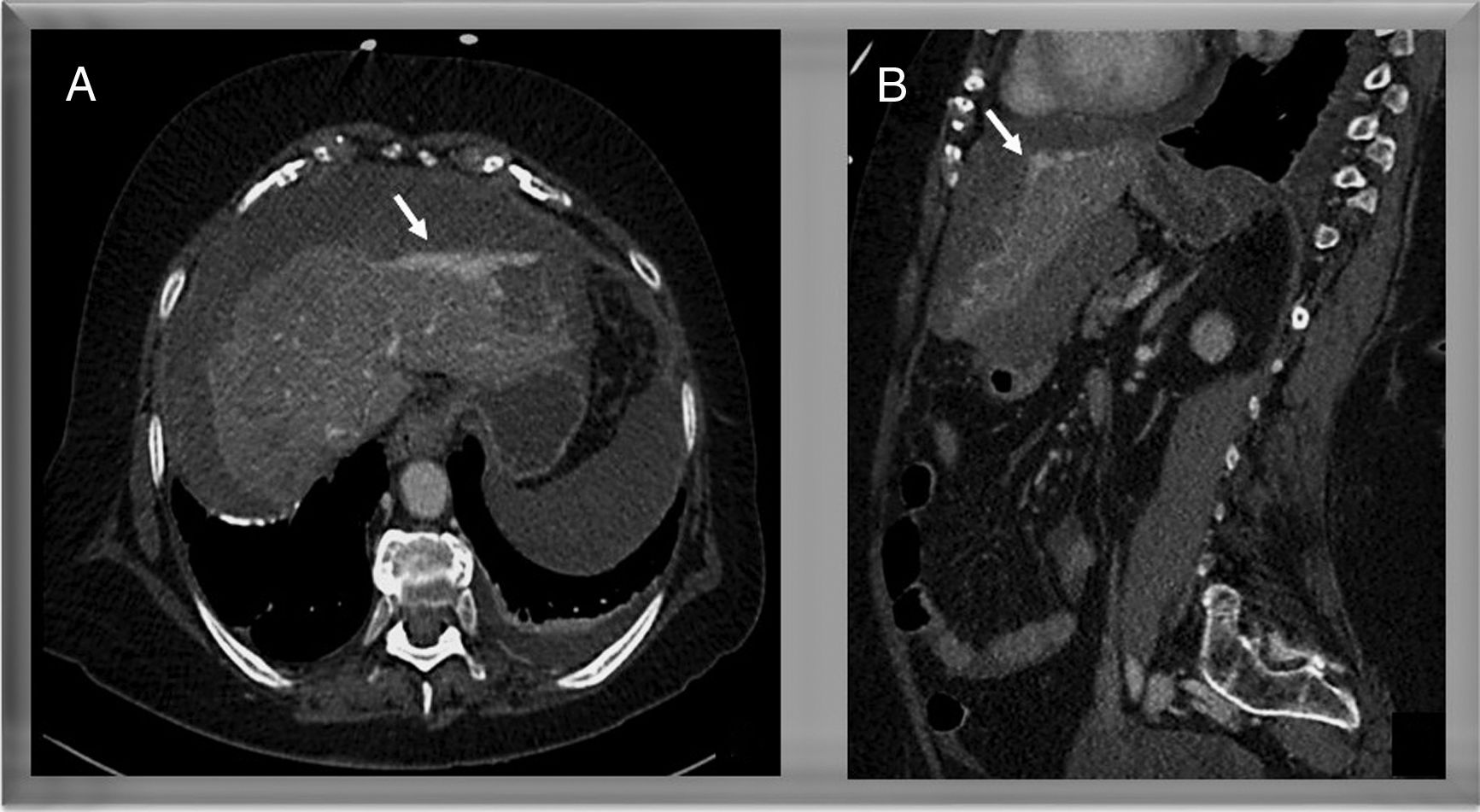
The second patient, an 85-year-old woman, was admitted to hospital presenting atrial flutter with a rapid ventricular response and symptoms of cardiac failure. Simultaneous treatment with low-molecular-weight heparin and warfarin was started with the objective of achieving an on-target international normalized ratio (INR) (Upon admission presented an INR of 1.19). The patient received a dose of 80mg of Enoxaparin BID and had a GFR of 56mL/min. After 48h of treatment, the patient presented syncope and hemodynamic instability (blood pressure (BP) 60/40mmHg). Blood tests revealed progressive anemia and acute kidney injury, as well as an INR of 4. Vasopressors were administered, and an emergency computed tomography scan revealed presence of a perihepatic hematoma (Fig. 2). The patient was taken to the operating room, where successful embolization of the left hepatic artery was performed by the interventional radiology team after correction of coagulopathy with fresh frozen plasma and prothrombin. After the procedure, the patient presented transitory improvement, with BP of 140/86mmHg. Minutes after leaving the operating room, however, the patient's hemodynamic status deteriorated again, with subsequent tests evidencing severe hypotension and worsening of anemia. An emergency exploratory laparotomy was ordered, evidencing presence of a hemoperitoneum of 2.5–3L and a hematoma in the left hepatic lobule. Hemostasis was achieved by manual compression. However, over the following hours the patient's situation worsened. She developed multiple organ dysfunction syndrome, which did not respond to treatment, eventually leading to death.
The prevalence of hemorrhagic complications of anticoagulant therapy has been reported at 5%, though this rate is greater in the case of elderly females.1 Most hemorrhagic events are intracranial, and the location of the two episodes presented here is relatively infrequent.2 The first is a muscular hematoma in the right psoas muscle (the most frequent site of muscular hematomas).1 These hematomas are usually produced through spontaneous bleeding and are associated with anticoagulant therapy.3 Large hematomas are rare, and can produce hemodynamic instability, in which case embolization is the procedure of choice.1
Diagnosis of hemorrhagic complications following anticoagulant therapy is challenging. Early clinical suspicion is critical. It is important to consider the characteristics of the patient and possible predisposing factors such as coagulopathy, advanced age, high BP, and diabetes mellitus, among others.1 Frequent signs and symptoms include pain at the site of bleeding and new or worsening anemia. Diagnosis is based on the findings of imaging tests, and computed tomography scan is the most sensitive method.2 In clinical practice, physicians must balance the thromboembolic risk with the hemorrhagic risk with respect to bridge therapy, considering the multiple adverse effects that have been previously described. Perhaps it is necessary to apply more discriminative scales of risk and to individualize this therapy according to the patient.4
Taking into account the potential life-threatening complications of anticoagulant therapy, we believe it is of vital importance that physicians become aware of the cases in which bridging therapy with low-molecular-weight heparin can be avoided.5 The decision to administer alternate therapy must be based on validated studies and follow the recommendations of scientific societies.6