Current guidelines establish an aortic valve area (AVA) cut-off point of <1cm2 for severe aortic stenosis; however, several studies suggest that a lower threshold area would better classify patients at risk. The aim of this study was to evaluate the outcome of patients with AS according to AVA.
MethodsA total of 140 patients with moderate-severe aortic stenosis and preserved ejection fraction were classified in three different groups according to baseline AVA. The outcomes (aortic valve intervention or all-cause mortality) were compared using Cox regression analysis.
ResultsAfter follow-up of 4.1 years (SD 1.9), death and/or aortic valve replacement occurred in 47 (84.1%) patients with AVA<0.75cm2, 48 (81.3%) with AVA 0.75–1cm2 and 15 (60%) with AVA>1cm2. Incidence of the combined endpoint was significantly higher in patients with AVA<0.75cm2 than AVA 0.75–1cm2 and AVA>1cm2 (4.71, 3.43 and 2.48 events per 100 person-years respectively) (P=.003). Survival differences stemmed only from the AVA <0.75cm2 group (HR, 1.58; P=.028 compared to the AVA 0.75–1cm2 group) with no differences between the 2 other groups (P=.117). Outcomes according to the indexed AVA (AVAi) were in accordance with the aforementioned results.
ConclusionsPatients with aortic stenosis and AVA between 0.75 and 1cm2 showed similar evolution to those with AVA>1cm2. However, those with AVA<0.75cm2 had a higher risk of complicated events. An AVA value <0.75cm2 would better distinguish patients at risk who might benefit from a more aggressive approach.
Las guías actuales de práctica clínica establecen el punto de corte del área valvular aórtica (AVA) en <1cm2 para la estenosis aórtica (EAo) grave; sin embargo, varios estudios sugieren que un punto de corte con un umbral más bajo clasificaría mejor a los pacientes en riesgo. El objetivo de este estudio fue evaluar la evolución de los pacientes con EAo según el AVA.
MétodosUn total de 140 pacientes con estenosis aórtica moderada-grave y fracción de eyección conservada se clasificaron en 3 grupos en función del AVA basal. Los resultados (intervención sobre la válvula aórtica o mortalidad global) se compararon mediante un análisis de regresión de Cox.
ResultadosTras un seguimiento de 4,1 años (DE 1,9), se produjo muerte o reemplazo valvular aórtico en 47 (84,1%) pacientes con AVA<0,75cm2, 48 (81,3%) con AVA 0,75-1cm2 y 15 (60%) con AVA>1cm2. La incidencia de la variable combinada fue significativamente mayor en pacientes con AVA<0,75cm2 que AVA 0,75-1cm2 y AVA>1cm2 (4,71, 3,43 y 2,48 eventos por 100 personas/año, respectivamente) (p=0,003). Las diferencias en las curvas de supervivencia provienen del grupo AVA<0,75cm2 (HR=1,58; p=0,028 en comparación con el grupo AVA 0,75-1cm2) sin hallarse diferencias entre los otros 2 grupos (p=0,117). Los resultados según el AVA indexada (AVAi) fueron equiparables con los resultados previamente mencionados.
ConclusionesLos pacientes con EAo y AVA entre 0,75 y 1cm2 mostraron una evolución similar a aquellos con AVA>1cm2. Sin embargo, aquellos con AVA<0,75cm2 mostraron un mayor riesgo de complicaciones. Un valor de AVA<0,75cm2 distinguiría mejor a los pacientes en riesgo que podrían beneficiarse de un enfoque más agresivo.
Aortic stenosis (AS) is the most common heart valve disease in western countries and its prevalence increases with age.1 Aortic valve replacement (AVR) or transcatheter aortic valve implantation (TAVI) are indicated when aortic stenosis is severe and presents with symptoms. However, symptoms in elderly patients with comorbidities are often not easy to assess; therefore, correct aortic stenosis severity grading is critical for deciding on surgical (or transcatheter) treatment. The cut-off values for severe aortic stenosis according to current guidelines when the ejection fraction (EF) is preserved (>50%) are aortic valve area (AVA)<1cm2 and mean aortic gradient>40mmHg.2,3 However, these values lead to discrepancies in AS classification in a high number of patients4–7 and several studies have questioned the consistency of these values, thereby suggesting that an AVA<1cm2 is not an adequate cut-off point. Carabello et al.8 suggested according to an invasive study that used the Gorlin equation that an average gradient of 40mmHg corresponds to an AVA of 0.8cm2. Minners et al. confirmed these data in an extensive series of AS patients also assessed by cardiac catheterisation and observed that 25% of the sample presented incongruent data.9 Furthermore, an AVA of 1cm2 correlated with a mean gradient of 22.8mmHg in vivo while a mean gradient of 40mmHg correlated with an AVA of 0.75cm2, and a maximum velocity of 4m/s with an AVA of 0.82cm2.7
Although incongruences related to aortic valve evaluation are well known, current clinical practice guidelines recommend sub-classifying AS with normal EF according to flow and gradient.2 Low flow is defined as the presence of an indexed stroke volume (SVi)≤35mL/m2. The low-flow low-gradient aortic stenosis first described in 2007 was considered a variant with worse prognosis compared to high-gradient AS.7 Since then, multiple studies had the common aim of determining the prevalence of this phenomenon and its clinical impact. Those studies had multiple limitations and results were heterogeneous8–12; however, most of them point to worse prognosis of this entity and consider the low-flow state a poor prognostic factor.
This study aimed to evaluate aortic valve replacement or mortality outcomes according to baseline AVA, indexed AVA (AVAi) and SVi in a cohort of patients with moderate-to-severe AS and preserved EF (>50%). The null hypothesis was that prognosis of patients with an AVA<0.75cm2 was similar to that of patients with an AVA 0.75–1cm2.
MethodsFrom 2010 to 2015, 668 consecutive adult patients (≥18 years) with significant aortic stenosis, including moderate and severe AS as defined by the current guidelines,2,3 and normal left ventricle EF underwent clinical evaluation and transthoracic echocardiography (TTE) at the outpatient clinic of a single tertiary referral centre. Patients were recruited irrespective of baseline symptomatic status. Subjects with atrial fibrillation, coronary artery disease (diagnosed by coronary angiography, positive ischaemia test or the presence of akinetic areas on the echocardiogram), more than mild mitral or aortic regurgitation, uncontrolled arterial hypertension and with suboptimal echocardiographic quality were excluded from the analysis. A total of 140 patients were included in the final study. Demographic and anthropometric data, TTE variables, pre-operative information, surgical details and last follow-up data (including clinical status) were retrospectively obtained from the patients’ records. The TTE records were analysed by an ESC-certified, experienced echocardiographer and the variables obtained were measured based on current echocardiography guidelines. Left ventricle diameters, volumes, left ventricle index mass and EF (Simpson's method), aortic valve disease severity parameters (AVA, AVAi, aortic jet velocity, mean gradient, dimensionless index), indexed stroke volume, left atrium diameter and area, E and A wave velocities and pulmonary artery systolic pressure were evaluated. Patients were classified in 3 groups according to AVA at diagnosis: AVA<0.75cm2, AVA 0.75–1cm2 and AVA>1cm2, and according to AVAi at diagnosis: AVAi<0.5cm2/m2, AVAi 0.5–0.59cm2/m2 and AVAi≥0.6cm2/m2. Patients were also divided according to indexed stroke volume: low flow if SVi≤35mL/m2 or normal flow if SVi>35mL/m2. All-cause mortality and aortic valve replacement were considered for the analysis. Causes of death were studied together with variables related to AVR (date, reasons for indication and type of AVR or TAVI). AVR was indicated according to the attending physician and the Heart Team final decision considering clinical status and echocardiography parameters. The protocol of our Department of Cardiology did not include AVA alone to define severity in patients with normal EF or indicate surgery. The Ethical Committee approved the study. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the institution's human research committee. Informed consent was not obtained because of the retrospective nature of the study (ethics committee approved it) and data were analyzed and treated anonymously.
All analyses were made using Software IBM SPSS statistics for Windows version 20 (IBM Corp., Armonk, United States). Continuous variables were expressed as mean and standard deviation (SD) and as median and interquartile range (Q1Q3). Normality of data was examined. If data conformed to normality, group comparisons were made by independent samples t test. If not, a nonparametric test was employed (Kruskal–Wallis). Categorical variables were expressed as percentages and compared by chi-square test or exact Fisher test, as appropriate. Associations between continuous variables were assessed by Pearson's test. Kaplan–Meier survival curves with log-rank test were also generated. Cox regression was used to compare in-between group differences. A two-tailed, P value<0.05 was regarded as statistically significant.
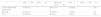
ResultsA total of 140 patients were recruited and classified in three groups: 56 in the group AVA <0.75cm2 (40%), 59 in the group AVA 0.75–1cm2 (42%) and 25 in the group AVA>1cm2 (18%). Mean follow-up of the whole cohort was 50 months (SD 23) with no differences among groups (P=.114). Mean age of the whole cohort was 76.3 years (SD 9.4), and the proportion of elderly patients (> 75 years) did not differ among groups. The proportion of females was significantly higher in the AVA<0.75cm2 group (P=.039) and body surface area also had significantly lower values (P=.047). Therefore, results were also analysed according to the AVAi. Baseline cardiovascular risk factors of patients were balanced as shown in Table 1.
Baseline demographic, clinical and echocardiographic parameters according to aortic valve area group.
| AVA<0.75cm2N=56 | AVA 0.75–1cm2N=59 | AVA>1cm2N=25 | P | |
|---|---|---|---|---|
| Demographic and clinical characteristics | ||||
| Follow-up, months | 46.4 (25.5) | 49.73 (20.6) | 57.9 (20.2) | .114 |
| Age, years | 77.8 (7.7) | 74 (10.8) | 78.5 (8.1) | .039 |
| Age>75 years, | 36 (64.3%) | 33 (55.9%) | 16 (64%) | .613 |
| Body surface area, kg/m2 | 1.6 (0.2) | 1.7 (0.2) | 1.8 (0.2) | .047 |
| Females | 40 (71.4%) | 37 (62.7%) | 10 (40%) | .026 |
| Hypertension | 45 (80.3%) | 44 (74.6%) | 21 (84%) | .576 |
| Dyslipidaemia | 31 (55.3%) | 29 (49.1%) | 15 (60%) | .622 |
| Diabetes | 20 (35.7%) | 13 (22%) | 10 (40%) | .153 |
| Baseline symptoms | 32 (57.1%) | 18 (31%) | 8 (32%) | .01 |
| Aortic stenosis echocardiographic parameters | ||||
| Aortic jet velocity, m/s | 4.3 (0.6) | 3.8 (0.6) | 3.5 (0.4) | <.0001 |
| Mean aortic gradient, mmHg | 48.5 (15.2) | 36.4 (12.5) | 29.5 (7.9) | <.0001 |
| Aortic valve area, cm2 | 0.56 (0.1) | 0.91 (0.1) | 1.27 (0.2) | <.0001 |
| Aortic valve area index, cm2/m2 | 0.34 (0.1) | 0.52 (0.1) | 0.72 (0.1) | <.0001 |
| Dimensionless index | 0.2 (0.1) | 0.28 (0.1) | 0.33 (0.1) | <.0001 |
| LVEF | 62.8 (6.7) | 63.4 (5.4) | 62.7 (5.5) | .847 |
| Indexed stroke volume, mL/m2 | 35.6 (13.2) | 42.9 (12.7) | 50.6 (19.3) | <.0001 |
| Myocardial mass, g | 226.8 (75.9) | 211.9 (61.1) | 231.8 (42) | .335 |
| IV septum, mm | 14.8 (2.7) | 14 (2.2) | 15.1 (2.2) | .113 |
| Posterior wall, mm | 12.3 (2) | 12 (2) | 12.8 (2) | .250 |
| LA diameter, mm | 42.4 (6.4) | 41.7 (6.2) | 42.6 (6.7) | .809 |
| LA area, cm2 | 23.3 (5.1) | 23.2 (4.4) | 24.1 (3.8) | .778 |
| E wave, cm/s | 0.8 (0.3) | 0.85 (0.3) | 0.79 (0.3) | .618 |
| A wave, cm/s | 1 (0.3) | 1.1 (0.4) | 1 (0.3) | .573 |
| PASP, mmHg | 36.8 (9.4) | 34 (7.7) | 40.7 (13) | .102 |
Data are expressed as no. (%) or mean±standard deviation. AVA, aortic valve area; LVEF, left ventricular ejection fraction; IV, interventricular; LA, left atrium; PASP, pulmonary artery systolic pressure.
As expected, the AVA groups had significantly different parameters of aortic stenosis severity (Table 1). Left ventricular EF, left ventricular wall thickness and myocardial mass were comparable among groups. AS severity assessment according to baseline AVAi subgroups also showed significant differences (Table 2).
Baseline echocardiographic parameters and symptomatic status according to index aortic valve area group.
| AVAi<0.5cm2/m2N=73 | AVAi 0.5–0.59cm2/m2N=29 | AVAi≥0.6cm2/m2N=29 | P | |
|---|---|---|---|---|
| Baseline symptoms | 34 (47) | 8 (29) | 11 (38) | .242 |
| Aortic jet velocity, m/s | 4.1 (0.7) | 3.8 (0.6) | 3.6 (0.5) | <.0001 |
| Mean aortic gradient, mmHg | 44.2 (14.8) | 36.5 (11.7) | 30.7 (11.4) | <.0001 |
| Aortic valve area, cm2 | 0.65 (0.17) | 0.93 (0.09) | 1.21 (0.20) | <.0001 |
| Aortic valve area index, cm2/m2 | 0.37 (0.08) | 0.55 (0.03) | 0.71 (0.09) | <.0001 |
| Dimensionless index | 0.22 (0.06) | 0.29 (0.05) | 0.34 (0.07) | <.0001 |
| LVEF, % | 63.4 (6.3) | 63.2 (5.9) | 63.1 (5.5) | .980 |
| Indexed stroke volume, mL/m2 | 38.4 (10.9) | 44.6 (9.7) | 54.3 (12.7) | <.0001 |
| Myocardial mass, g | 224.9 (72.1) | 210.7 (66.8) | 222.6 (48.1) | .629 |
| IV septum, mm | 14.4 (2.6) | 14.5 (2.5) | 14.6 (2.3) | .966 |
| Posterior wall, mm | 12.2 (1.9) | 12 (2.3) | 12.6 (2) | .535 |
| LA diameter, mm | 42.4 (6.4) | 41.9 (5.4) | 41.0 (7.3) | .642 |
| LA area, cm2 | 23.8 (5.1) | 23.3 (3.6) | 22.1 (4.7) | .360 |
| E wave, cm/s | 0.79 (0.3) | 0.92 (0.4) | 0.78 (0.3) | .133 |
| A wave, cm/s | 1 (0.4) | 1.1 (0.3) | 1 (0.3) | .647 |
| PASP, mmHg | 35.5 (9.1) | 35.8 (7.9) | 39.6 (13.6) | .398 |
Data are expressed as mean±standard deviation. AVAi: indexed aortic valve area; LVEF: left ventricular ejection fraction; IV: interventricular; LA: left atrium; PASP: pulmonary artery systolic pressure.
At the initial evaluation, 64 (45.7%) patients were symptomatic: 50 (36%) presented dyspnoea, 10 (7.2%) angina pectoris and 4 (2.9%) syncope. Baseline symptoms were significantly more frequent in the AVA group <0.75cm2 (32, 57%) compared to the AVA group 0.75–1cm2 (18, 31%) and the AVA group> 1cm2 (8, 32%) (P=.01) (Table 1 and Table 3). Symptomatic patients showed lower AVAi compared to asymptomatic patients (P=.009) (Table 3). Although there was a trend among patients with AVAi<0.5cm2/m2 to be more symptomatic, differences according to AVAi subgroup were non-significant (P=.242) (Table 2). Symptoms did correlate with myocardial wall thickness, relative wall thickness and both global and indexed myocardial mass. Echocardiographic parameters according to symptomatic status are shown in Table 3.
Echocardiographic parameters according to the symptomatic status.
| Presence of symptomsN=64 (46%) | Absence of symptomsN=76 (54%) | P | |
|---|---|---|---|
| Myocardial mass, g (SD) | 244.1 (75.6) | 203.7 (49.5) | <.0001 |
| Myocardial mass indexed, g/m2 (SD) | 141.8 (43.3) | 119.5 (29.1) | .001 |
| IV septum, mm (SD) | 15.2 (2.8) | 14.1 (2) | .006 |
| Posterior wall, mm (SD) | 12.9 (1.9) | 11.7 (1.9) | <.0001 |
| LA diameter, mm (SD) | 43.4 (6.2) | 41.2 (6.3) | .057 |
| Relative wall thickness (SD) | 0.58 (0.12) | 0.53 (0.11) | .020 |
| LA area, cm2(SD) | 23.9 (4.7) | 23.03 (4.7) | .356 |
| E wave, cm/s (SD) | 0.84 (0.3) | 0.79 (0.3) | .474 |
| A wave, cm/s (SD) | 1.06 (0.3) | 1.04 (0.4) | .795 |
| PASP, mmHg (SD) | 38.03 (9.6) | 35.4 (10) | .263 |
| AVA, cm2(SD) | 0.76 (0.15) | 0.89 (0.28) | .008 |
| AVAi, cm2/m2 (SD) | 0.44 (0.15) | 0.52 (0.16) | .009 |
Data are expressed as mean±standard deviation. AVA, aortic valve area; AVAi, indexed aortic valve area; IV: interventricular; LA: left atrium; PASP: pulmonary artery systolic pressure.
72 patients (51%) underwent AVR with an incidence rate of 4.08 (95%CI, 3.22–5.18) surgeries per 100 person-years. The reason for AVR was dyspnoea and/or heart failure in 56 patients (78% of AVR), angina pectoris in 6 (8%), syncope in 1 (1%), rapid progression of AS severity in 3 (4%) and other causes in 6 (8%). At the time of AVR, all patients fulfilled criteria of severe AS, including those with initial AVA>1cm2, who showed an expected progression of AS severity during follow-up (Table 1 of the supplementary data).
All-cause mortality and aortic valve replacement outcomes according to aortic valve areaA total of 50 deaths (35.7%) occurred during follow-up with an incidence rate of 2.97 (95%CI, 2.25–3.92) deaths per 100 person-years. Only 14 (28%) of those were clearly related to cardiovascular causes, including 3 patients who died in the postoperative period and 1 who died from heart failure after palliative valvuloplasty. 25 patients (50%) died from non-cardiovascular causes and the cause of death could not be determined in 11 patients (22%). 72 patients (51%) underwent AVR. 12 (16.7%) died after AVR.
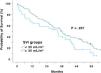
Although the proportion of cardiac events during follow-up differed slightly among groups due to natural progression of the valve disease, the incidence rate of the endpoint was significantly higher in the AVA<0.75cm2 group (4.71, 95%CI, 3.50–6.36, events per 100 person-years) compared to the AVA 0.75–1cm2 (3.43, 95%CI, 2.58–4.55, events per 100 person-years) and AVA>1cm2 (2.48; 95%CI, 1.49–4.11, events per 100 person-years) groups (log-rank test P=.003, Table 4, Fig. 1). Survival curves differences stemmed only from the AVA <0.75cm2 group (HR, 1.58; 95%CI, 1.05–2.37; Cox regression P=.028 compared to AVA 0.75–1cm2 group), with no differences between the two latter groups (HR, 0.623; 95%CI, 0.35–1.13; Cox regression P=.117, group AVA>1cm2 compared to group AVA 0.75–1cm2).
Rates of mortality and/or AVR, mortality alone and AVR alone in the different AVA groups.
| AVA<0.75cm2N=56 | AVA 0.75–1cm2N=59 | AVA>1cm2N=25 | P | |
|---|---|---|---|---|
| Total events (death and/or AVR) | 47 (84.1%) | 48 (81.3%) | 15 (60%) | .042 |
| Mortality | 22 (39.3%) | 18 (30.5%) | 10 (40%) | .547 |
| AVR | 30 (53.6%) | 36 (61%) | 6 (24%) | .007 |
Data are expressed as no. (%). AVA, aortic valve area; AVAi, indexed aortic valve area; AVR, aortic valve replacement.
Although a trend for overall mortality to occur earlier was observed in patients with more severe AS, no significant differences for mortality among groups were found (log-rank test P=.165) (Table 4). Surgery was performed earlier in the AVA<0.75cm2 group (6.57 events per 100 person-years) than in the AVA 0.75–1cm2 group (3.51 events per 100 person-years) and AVA>1cm2 group (2.46 events per 100 person-years) (log-rank test P<.0001) (Table 4). Differences were only due to an earlier indication in the AVA group<0.75cm2 (HR, 2.60; 95%CI, 1.55–4.36, Cox regression P<.0001 compared to the AVA group 0.75–1cm2), with no differences between the AVA 0.75–1cm2 and AVA>1cm2 curves (HR, 0.60; 95%CI, 0.25–1.44, Cox regression P=.252, group AVA>1cm2 compared to group AVA 0.75–1cm2).
All-cause mortality and aortic valve replacement outcomes according to indexed aortic valve areaResults according to AVAi groups were superimposable (Table 5, Fig. 1 of the supplementary data). The proportion of cardiac events during follow-up differed slightly among groups but survival curves showed significant differences (log-rank test P=.002 for AVR and/or death). Risk of events was higher in the AVAi<0.5cm2/m2 group (HR, 2.03; 95%CI, 1.27–3.23; Cox regression P=.003 compared to AVAi 0.5–0.59cm2/m2), mainly due to an earlier surgery indication (HR, 2.84; 95%CI, 1.56–5.14; Cox regression P=.001 compared to AVAi 0.5–0.59cm2/m2) and with no differences in mortality (log-rank test P=.152). Results between AVAi 0.5–0.59cm2/m2 and AVAi≥0.6cm2/m2 were similar (HR, 1.02; 95%CI, 0.55–1.91; Cox regression P=.949 for the combined endpoint).
Rates of mortality and/or AVR, mortality alone and AVR alone in the different AVAi groups.
| AVAi<0.5cm2/m2N=73 | AVAi 0.5–0.59cm2/m2N=29 | AVAi≥0.6cm2/m2N=29 | P | |
|---|---|---|---|---|
| Total events (death and/or AVR) | 61 (83.6%) | 27 (93.1%) | 16 (55.2%) | .001 |
| Mortality | 27 (37.0%) | 11 (37.9%) | 9 (31%) | .824 |
| AVR | 42 (57.5%) | 18 (62.1%) | 9 (31.0%) | .028 |
Data expressed as number (percentage). AVA, aortic valve area; AVAi, indexed aortic valve area; AVR, aortic valve replacement.
Low flow was present in 36 (27.5%) patients and normal flow in 95 (72.5%). Correlation between myocardial mass and SVi was poor (r=0.032; P=.711). All-cause mortality or AVR occurred in 30 (83%) patients in the low-flow group and in 73 (77%) in the normal-flow group, with no significant differences between groups (log-rank test P=.207) (Fig. 2). No differences in mortality (log-rank test P=.395) or AVR (log-rank test P=.132) were observed among groups. When AVA and SVi
parameters were combined, differences in mortality and/or AVR among groups were also non-significant (log-rank test P=.304) (Fig. 2 of the supplementary data).
DiscussionThis series comprises a consecutive cohort of 140 patients presenting moderate to severe AS and preserved EF with similar cardiovascular risk factors and without evidence of ischemic heart disease managed at a single centre according to a pre-established protocol with a mean follow up of 4 years. Remarkably, the number of events was high regardless of AS severity and the presence of symptoms at diagnosis, with 78.6% mortality and aortic valve intervention.
Regarding AS severity assessment, the mean values of other AS severity parameters in the AVA group 0.75–1cm2 resemble moderate AS values. Discrepancies arose when AS severity was assessed in multiple series using echocardiography, catheterisation,7,9,10 MRI5,11 and CT.12 The main factor underlying this inconsistent grading is underestimation of the SVi due to the assumption of circular geometry of the left ventricle outflow tract when two-dimensional TTE is used.13 Studies using three-dimensional techniques (CT, CMR or 3D-echocardiography) have shown that the introduction of the planimetered left ventricle outflow tract area into the continuity equation yields significantly larger aortic valve areas and this leads to severe AS patients being re-classified as moderate in 20–55% of cases.5,12,14 In this series and most of the published ones, left outflow tract diameter was assessed by two-dimensional TTE and thus systematic underestimation of the AVA was to be expected. A lower AVA cut-off point would reduce these discrepancies.
The presence of symptoms in severe AS with preserved ejection fraction is a class IB indication of aortic valve replacement according to current guidelines. Nonetheless, symptoms in elderly patients, with hypertension and other comorbidities, can be difficult to determine except when an exercise test can be performed. As expected, in this series, symptoms at the time of diagnosis were more frequent in patients with AVA<0.75cm2, while symptoms in patients with AVA 0.75–1cm2 and moderate aortic stenosis (AVA>1cm2) did not differ. Symptoms did correlate with hypertrophy (myocardial wall thickness and myocardial mass) but not with other parameters.
Although current guidelines consider the AVA to be one of the pivotal points indicating AS severity or AVR, series that studied the natural history of this valve disease with normal EF historically found maximum aortic valve velocity but not the aortic valve area to be one of the main prognostic factors.15–17 In the present series, patients with AVA<0.75cm2 and a high gradient (>40mmHg) had higher risk of death and/or AVR than the other groups, although the number of events was comparable among AVA groups due to progression of aortic stenosis severity in all groups. Although overall mortality did not differ between groups, death tended to occur earlier in patients with more severe AS according to the AVA. Surgery was performed earlier in the AVA<0.75cm2 group than in the AVA 0.75–1cm2 and AVA>1cm2 groups. Although AVA may be the cornerstone of the algorithm decision at some centres, at our centre, maximum velocity and gradients, symptoms and other diagnostic tests (exercise test, calcium load assessment) were historically considered ahead of the area owing to the widely known limitations of the continuity equation. However, as in previous published studies, the indication of AVR depends on the responsible physician, so despite being considered a major event, it should always be interpreted with caution. Although patients in our intermediate group (AVA 0.75–1cm2) could be considered to have severe stenosis according to the guidelines, they had a less aggressive profile and, although they underwent AVR less frequently, they did not present a higher mortality rate. In fact, in our population, an AVA cut-off point of 1cm2 would determine a high number of false-positive cases and thus integration of other severity parameters (transoesophageal AVA planimetry, valve calcium load, etc.) would be needed.
Several authors suggest using the indexed AVA because some discrepancies could be secondary to variations in body surface area among different populations. An indexed AVA<0.5cm2/m2 was suggested to be a valid cut-off point for severe AS.18 In the present series, the AVA group<0.75cm2 had a higher proportion of women and this factor probably contributed to the smaller body surface areas in this group. All the analyses of the study were also made according to the indexed AVA and the results were comparable to those with the non-indexed AVA, with an 0.5cm2/m2 cut-off point being established for the lowest AVA group. Correction for body surface area did not improve the grading of AS in other series7 and was considered to significantly increase the prevalence of patients with criteria for severe AS by including patients with a milder degree of the disease without improving predictive accuracy for aortic valve-related events.18 In fact, in our series, AVAi<0.5cm2/m2 seemed a less strict criterion than AVA<0.75cm2, showing lower values of aortic mean gradient, maximum velocity and dimensionless index than in the non-indexed group. Nevertheless, as part of AS evaluation, AVAi should always be considered in smaller subjects.
Hachicha et al. first described the presence of low stroke volume (SVi≤35mL/m2) in patients with AS despite normal EF and its association with poorer outcome.19 The reported prognostic value of this phenomenon varies widely among different series. Several studies obtained similar results with worse outcome in patients with low-flow low-gradient AS compared to high-gradient AS,20–23 thereby considering it a more advanced stage of the disease. Low-flow has also been shown to be a major predictor of perioperative mortality,24 overall mortality in extensive series25 and an independent predictor of mortality, regardless of EF.26 However, results of other studies differed. In a series of 1525 patients with AS, Jander et al. observed that reduced stroke volume index was not associated with more valve-related events.27 Similar results are also described by other authors who observed behavior similar to moderate AS,4 and recent meta-analyses do not support the theory of worse outcome for this group of patients or a greater need for AVR.28,29 In this study, prognostic differences were not detected between patients with high or low flow. A significant but weak correlation was also found between AVA and SVi, probably secondary to the same methodology used to calculate both equations that contain the same source of error, i.e. outflow tract diameter measurement. Interestingly, although a low-flow state in severe AS was associated in different series with a higher prevalence of hypertension and myocardial mass, we found no correlation between SVi and myocardial mass.30
Study limitationsThe main limitation of this study was its retrospective nature. Although the series did not comprise a high number of patients, the sample was very homogeneous, from a single center and patient management followed well-defined and established protocols.
The vast majority of studies evaluating AS severity parameters in recent decades consider AVR to be part of AS prognosis, although the indication for surgery obviously depends on these parameters. However, studies evaluating the true natural history of the disease seem difficult to conduct owing to guideline indications and the difficulty in assessing symptoms in this population. In this series, the attending physicians considered mean aortic gradient rather than AVA to indicate intervention in symptomatic patients. AVA was only used when systolic dysfunction or hyperkinetic factors were present. Only 18% of patients in our series had moderate AS (AVA>1cm2), probably due to selection bias of a tertiary hospital and the less severe form of the disease; however, we considered it representative of moderate AS in our population.
In the majority of patients in this cohort, low-flow status could not be validated by other imaging techniques (3D echocardiography, CT, MRI). Nevertheless, as most studies evaluating AS prognosis are based on echocardiography, results comparable to those of our study can be assumed.
Conclusions are based on mortality and AVR, as in the majority of previous published studies. However, the indication of AVR depends on the responsible physician. In our centre, AVR was indicated according to the attending physician and the Heart Team final decision considering clinical status and echocardiography parameters, according to a robust protocol that did not include AVA alone to define severity but considering other multiple factors. Moreover, conclusions are especially based on the time to event, since the difference in the number of events is limited by the number of patients of this study.
ConclusionsAmong patients with AS and AVA<1cm2, those with AVA between 0.75cm2 and 1cm2 had a similar evolution to those with AVA>1cm2. However, those with AVA<0.75cm2 had an earlier and higher risk of complicated events. An AVA value<0.75cm2 would better distinguish patients at risk who might benefit from a more aggressive approach. Therefore, a small AVA of ≤1.0cm2 alone should not be used as a single parameter for the diagnosis of severe AS. In patients with AVA between 0.75 and 1cm2, integrated evaluation using multimodality imaging and biomarkers is required to determine the true severity of AS.
- -
Aortic stenosis classification according to guidelines lead to discrepancies in a high number of patients and several studies have questioned the consistency of these values.
- -
Current guidelines establish an aortic valve area cut-off point of <1cm2 for severe aortic stenosis; however, several studies suggest that a lower threshold area would better classify patients at risk.
- -
After 4 years of follow-up, high death and/or AVR rates were observed in the whole cohort. Although differences among groups were slight, median time to the combined endpoint was significantly shorter in patients with AVA<0.75cm2 than with AVA 0.75–1cm2 and AVA>1cm2.
- -
Survival differences stemmed only from the AVA<0.75cm2 group. We conclude that patients with aortic stenosis and AVA between 0.75 and 1cm2 showed similar evolution to those with AVA>1cm2; however, those with AVA<0.75cm2 had a higher risk of complicated events.
The authors received no specific funding for this work.
Authors’ contributionL. Galian, G. Casas, and A. Evangelista designed the study. G. Casas, L. Galian-Gay, C. Granato and R. Fernández-Galera collected the data and drafted the document. A. Sao Avilés, G. Teixidó, A. Guala and A. Ruiz analyzed the data. A. Evangelista, J. F. Rodríguez-Palomares and T. González-Alujas reviewed the collected data and revised the drafting of the final document. L. Gutierrez and F. Valente contributed to the elaboration of the final manuscript.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors wish to thank Christine O’Hara for her help with the English version of the manuscript.
Abbreviations: AVA: aortic valve area; AVAi: indexed aortic valve area; AS: aortic stenosis; AVR: aortic valve replacement; EF: ejection fraction; SVi: indexed stroke volume.