The clinical impact of the systems for rapid access to reperfusion therapy for patients with ST-segment elevation myocardial infarction (STEMI) has not been definitely established. The aim of this study is to investigate the effect on short term mortality of a myocardial infarction network organization (MINO).
MethodsA prospective single-center cohort study was designed, including all patients who met the following criteria: chest pain, less than 12h since symptoms onset, and ST-segment elevation in at least 2 contiguous leads on the electrocardiogram.
ResultsA total of 594 patients were included. MINO patients had both lower time since symptoms onset and lower time from arrival at the hospital to guidewire introduction in the culprit coronary artery: median of 190min [IQR 130/270] vs 258min [IQR 165/420] P<.001 and 33min [IQR 25/41] vs 78min [IQR 60/128] P<.001, respectively. Heart failure was higher in the non-MINO group: Killip class >1 was detected in 36.4% vs 25.28%, respectively, P=.076. There were 45 deaths during 30-day follow-up, 5.6% in the MINO group vs 10.7%. Patients using MINO had better mid-term survival, log-rank test=5.41, P=.02. However, in the multivariable Cox proportional hazard analysis, it was not associated with total mortality, HR,0.71 (0.39–1.36).
ConclusionsIn patients with STEMI, the set-up of a system to provide rapid reperfusion reduces the time to the opening of the culprit coronary artery. However, we did not find any difference in 30-day mortality rate in multivariable models.
El impacto clínico de los sistemas para el acceso rápido al tratamiento de reperfusión en pacientes con infarto de miocardio con elevación del segmento ST (IAMCEST) no está del todo establecido. El objetivo de este estudio fue estudiar el efecto en la mortalidad a corto plazo de la implementación del código infarto (CI).
MétodosEstudio de cohortes, unicéntrico, en el que se incluyó a todos los pacientes que cumplían los siguientes criterios: dolor torácico, menos de 12h de inicio y elevación del segmento ST en al menos 2 derivaciones continuas del electrocardiograma.
ResultadosSe incluyeron 594 pacientes. El grupo CI presentó tiempos menores desde el inicio de los síntomas a la llegada del hospital y a la introducción de la guía en la arteria responsable: media de 190min [IQR 130/270] frente a 258min [IQR 165/240] p<0,001 y 33min [IQR 25/41] frente a 78min [IQR 60/128] p<0,001. La clase Killip>I se dio en el 36,4% del grupo no CI frente al 25,28%; p=0,076. Hubo 45 muertes durante el seguimiento: 5,6% en el grupo CI frente al 10,7%. El uso del CI se asoció a una mejor supervivencia a corto plazo, test de log rank=5,41; p=0,02; no obstante, en el análisis multivariante de Cox no hubo diferencias en la mortalidad total, HR=0,71 (0,39-1,36).
ConclusionesLa implementación de un sistema de rápido acceso a la reperfusión en el IAMCEST reduce el tiempo hasta la apertura de la arteria responsable. Sin embargo, en el análisis multivariante, no hubo diferencias en la mortalidad a 30 días.
The benefits of early reperfusion in patients presenting with ST-segment elevation myocardial infarction are well established.1–3 Rapid access to the treatment increases its efficacy and decreases morbidity and mortality.4 For this reason, it is of paramount importance to facilitate the arrival of the patients with an acute coronary syndrome to a medical center as soon as possible, thereby providing the reperfusion treatment in accordance to the current guidelines for clinical practice.5,6 With this goal, some institutions have set up a network to attend ST-segment elevation myocardial infarction (STEMI) shortening the time to reperfusion either with out-of-hospital fibrinolysis combined with coronary angioplasty as required (pharmacoinvasive strategy) or with primary percutaneous coronary intervention (PCI) transferring the patient to a nearby hospital with a catheterization laboratory.7,8
Clinical trials designed to evaluate the best reperfusion strategy, either on-site or transferred to the nearest hospital with a primary PCI program have reported compelling conclusions. Immediate fibrinolysis in case of fewer than 3h since symptoms onset with rescue angioplasty if needed or primary angioplasty for the treatment of acute ST segment myocardial infarction have similar results, as reported in the PRAGUE-2, STREAM, and DANAMI-II studies as well as in registries such as FAST-MI.1,3,9,10 They have provided evidence of the safety of transporting patients from regional hospital to the PCI capable hospital.
The implementation of this type of organizational systems in “real life” has been reported. As cited by Kristensen et al.11 these networks have increased the rate of primary PCI with a reduction in time to reperfusion with the consequent widespread in its use. Some other studies, such that by Jollis et al.7 report a slight but significant increase in patients meeting the guidelines recommendations.
However, an analysis of the efficacy of these systems in real life should ideally be done after its implementation and not before and after its application, since not all the patients with symptoms suggestive of myocardial infarction reach the first medical contact using the system, and pre- and post-studies have intrinsic biases that preclude definite conclusions on the impact of the system on clinical endpoints.
The myocardial infarction network organization (MINO) emerged in our region in 2014 as an effort to provide patients undergoing STEMI timely reperfusion treatment according to the recommendations in the current guidelines5,6 through a single phone call made by the first medical contact to activate the catheterization laboratory and bypassing the emergency department.
So far, the published studies have evaluated the rapid access to the health care system, usually at two different periods of time: before and after its implementation.7,9,12 Our study aimed to investigate whether the patients who use the MINO are different from the patients who came to our institution by their own means as well as the relationship with short-term overall mortality. We hypothesized that the system reduces overall mortality rate at 30 days after the index STEMI.
MethodsWe designed an observational prospective cohort study. All patients who met the following criteria were included in the study: non-traumatic chest pain or discomfort, less than 12h since symptoms onset, and ST-segment elevation in at least 2 contiguous leads on the electrocardiogram. Only those patients who died before making the electrocardiogram were excluded. Those patients who had a resuscitated cardiac arrest as the first clinical manifestation of the infarct were not excluded from the study.
All the clinical data of the patients were collected on admission after clinical stabilization. Patients could arrive at the hospital in 2 ways: a) directly to the emergency room by their own means or in a general ambulance after contacting their general practitioners and b) after a specific phone call made by a health care professional or by the patients, which activates the MINO (Fig. 1).
According to the Spanish Statistical Office, the population density in our community was 26km2 in 2016. Our institution is the only PCI-capable hospital in the province, being the referral center for 2 non-PCI-capable hospitals, whose distance are 80km and 125km, respectively. Hence, our referral population is 550,000 inhabitants.
Two types of codes comprised the MINO: Type I, for patients who can be transferred in less than 120min of the first medical contact, and are intended for primary PCI; and Type II, for patients whose transportat would take more than 120min and thus received fibrinolysis as a reperfusion therapy, followed by an immediate transfer to the hospital with primary angioplasty 24/7. Those patients could have rescue angioplasty if on arrival there was clinical or electrical evidence of evolving ischemia or routine coronary angiogram in the first 24h after fibrinolysis, if reperfusion criteria were met at admission.
In our institution, all patients presented directly to our emergency services meeting the abovementioned inclusion criteria are treated with primary PCI. As such, all patients who came to the hospital by their own means or referred from a general practitioner were treated with a primary PCI.
The recruitment period spanned from February 2015 to June 2017. Baseline characteristics and data derived from the intervention were collected at the time of admission or during the patient's hospitalization. Patients were contacted 30 days after the index STEMI, either in a specific outpatient clinic or by phone.
Based on the results of the study of Cequier et al.8 and on our own previous surveillance of the results of the MINO program, the expected relative reduction in mortality at 30 days in the MINO group compared with the control will be 60%. Assuming that 40% of patients use the MINO to reach the hospital and a mortality rate of 12% in the control group, for an alpha error of 0.05 and a statistical power of 0.8, at least 512 patients would be needed to obtain a significant difference. To avert potential biases inherent to the study design, we took care to recruit consecutive patients and we report the results of both bivariate and multivariate analyses to account for the expected baseline differences between both groups.
For this paper, all patients were included in the analysis and we did not parse any subgroup gleaned from the whole database. Continuous variables are shown as mean and standard deviation in parentheses or median and interquartile range in case they did not fit a normal distribution (Shapiro–Wilks test). A log-transformation was done in the latter case if necessary, re-checking the adjustment to a normal distribution. Categorial variables are shown as number and percentage in parenthesis. Comparison between continuous variables was made with the Student t test and between categorical variables with the Chi-square test without continuity correction. Survival was analyzed with the Kaplan Meier curves and comparison between survival curves was done with the log-rank (Mantel-Haenszel) test. A multivariable Cox proportional hazard model was done to assess the efficacy in reducing total mortality with the MINO, adding all these potential confounding factors to the model (age, sex, diabetes mellitus, previous myocardial infarction, percutaneous intervention performed, anterior vs. non-anterior myocardial infarction, Killip class, cardiac arrest, and glomerular filtration rate). The assumption in the Cox model of proportional hazards with time was checked. A P value<.05 was considered significant.
For missing baseline categorical variables, we imputed using k-nearest-neighbor (k-NN) with a k value of 5. For continuous variables, we used the same method imputing the median of the closest five cases. We imputed one case of the variable “previous cerebrovascular accident” and 60 cases (10%) of “modification of diet in renal disease (MDRD) at admission” which is a non-negligible proportion. A sensitivity analysis was performed, reporting the result of the multivariable Cox regression model with the complete cases dataset on the primary endpoint of the study.
The primary endpoint of the study was total mortality at 30 days after the index myocardial infarction.
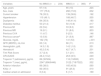
ResultsFrom February 2015 to June 2017, 607 patients were eligible for our study. Nonetheless, 13 patients had to be excluded: 7 refused to sign consent and 6 did not undergone primary PCI; therefore 594 patients were included in the study, 360 (60.6%) used the MINO to reach to the hospital. The baseline characteristics of the patients are depicted in Table 1. Patients in the MINO group had a significantly lower prevalence of diabetes mellitus. As such, the MINO group had lower glucose levels on admission. The glomerular filtration rate was statistically higher in the MINO group, with a mean difference between the groups of 2.7mL/min [95% confidence interval (95%CI) 0.6-4.9; P=.013]. As an overall assessment of the risk associated with the myocardial infarction, the TIMI risk score for STEMI was lower in the MINO group, with a mean absolute reduction of 0.6, (95%CI 0.2-0.9; P=.004), as it was the bleeding risk score CRUSADE: absolute mean reduction of 1.7, 95%CI 0.01-3.5; P=.049. We did not find any other statistically significant difference in the rest of the baseline variables. Thirty-two patients were treated with a fibrinolytic agent as the first reperfusion strategy, most of them in the MINO group [30 (8.5%) vs. 2 (0.8%), P<.001]. All the patients in the MINO group who received fibrinolysis as a reperfusion therapy, presented to a secondary hospital and they were transferred to our hospital. A total of 23 (71.9%) of these patients (all in the MINO group) had a rescue angioplasty due to failed reperfusion 90min after the drug administration.
Baseline characteristics.
| Variables | No MINO (n=234) | MINO (n=360) | P |
|---|---|---|---|
| Age, years | 67 (14) | 65 (13) | .224 |
| Sex, male | 177 (75.6) | 266 (73.9) | .632 |
| Current smoker | 78 (33.3) | 139 (38.6) | .192 |
| Hypertension | 115 (49.1) | 168 (46.7) | .555 |
| Dyslipemia | 84 (35.9) | 149 (41.4) | .180 |
| Diabetes mellitus | 50 (21.4) | 50 (13.9) | .017 |
| Previous MI | 22 (9.4) | 33 (9.2) | .923 |
| Previous MR | 19 (8.1) | 31 (8.6) | .833 |
| Previous CVA | 11 (4.7) | 9 (2.5) | .146 |
| Previous cancera | 13 (5.6) | 21 (5.8) | .887 |
| Glucose, mg/dL | 162 (76) | 141 (53) | <.001 |
| GFR (MDRD), mL/min | 63 (14) | 66 (11) | .013 |
| Hemoglobin, g/dL | 14.3 (1.9) | 14.2 (1.8) | .551 |
| Hematocrit | 43.2 (5.4) | 42.7 (4.7) | .201 |
| Timi Risk Score | 3.7 (2.4) | 3.1 (2.1) | .004 |
| CRUSADE | 28.4 (10.2) | 26.6 (9.5) | .049 |
| Troponin T (admission), pg/mL | 89 (30/504) | 118 (19/693) | .973 |
| Troponin T (max), pg/mL | 2547 (896/6446) | 3122 (718/7322) | .552 |
| Anterior infarction | 89 (38.0) | 165 (45.8) | .060 |
| Killip >1 | 82 (35.0) | 91 (25.3) | .010 |
| Cardiac arrest on admission | 8 (3.4) | 6 (1.7) | .169 |
CVA, cerebrovascular accident; GFR, glomerular filtration rate; MI, myocardial infarction; MINO, myocardial infarction network organization; MR, myocardial revascularization.
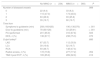
There were striking differences in the time elapsed from symptoms onset to the introduction of the guidewire in the culprit coronary artery, with a difference in median time of 68min in favor of the MINO group. The difference was also significant for the time from arrival at the hospital to guidewire introduction: 45min, both statistically significant (Table 2).
Results of the invasive procedures performed.
| No MINO (n=234) | MINO (n=360) | P | |
|---|---|---|---|
| Number of diseased vessels | .989 | ||
| 0 | 22 (9.4) | 33 (9.2) | |
| 1 | 110 (47.0) | 174 (48.3) | |
| 2 | 63 (26.9) | 93 (25.8) | |
| 3 | 39 (16.7) | 60 (16.7) | |
| Time from | |||
| Symptoms to guidewire (min) | 258 (165/420) | 190 (130/270) | < .001 |
| Door to guidewire (min) | 78 (60/128) | 33 (25/41) | < .001 |
| PCI performed | 201 (85.9) | 316 (87.8) | .505 |
| DES, n (%) | 136 (67.7) | 238 (75.3) | .070 |
| Culprit arterya | .680 | ||
| LAD | 67 (33.7) | 112 (35.9) | |
| LCx | 39 (19.6) | 52 (16.7) | |
| RCA | 93 (46.7) | 148 (47.4) | |
| Radial access, n (%) | 172 (73.8) | 277 (77.2) | .354 |
| TIMI 3 post PCIb, n (%) | 165 (85.9) | 289 (92.9) | .010 |
DES, drug eluting stent; LAD, left anterior descending artery; LCx, left circumflex; MINO, myocardial infarction network organization; PCI, percutaneous coronary intervention; RCA; right coronary artery.
More patients in the group which used MINO had an anterior myocardial infarction: [89 (38.0%) vs. 165 (45.8%), P=.060], although the difference did not reach statistical significance, and the percentage of patients with signs of heart failure were numerically lower in the MINO group. As such, a Killip class >1 was diagnosed in the non-MINO group 82 (35.0%) vs. 91 (25.3%) in the MINO group, P=.010. The success rate of the primary PCI, evaluated by the TIMI flow 3 after the procedure, was significantly higher in the MINO group:289 (92.9%) vs. 165 (85.9%) P=.010.
Survival analysisNo patient was lost during follow-up. There were 45 (7.8%) deaths during the 30-day follow-up, 20 (5.6%) in the MINO group and 25 (10.7%) in patients who reach the hospital by their own means log-rank test=5.41, P=.020, (Fig. 2). The relative hazard ratio (HR) reduction was 52% (Table 3 for the results of the univariate analyses). In Table 3 the data gleaned from the multivariable Cox proportional hazard analysis with the potential confounders is shown. In this latter analysis, the method used by the patient to arrive to the hospital was no longer associated with overall mortality at 30 days: HR,0.71 (0.39–1.32). We did not detect an interaction with time (P=.745).
Univariate and multivariate (Cox regression) analysis to predict 30-day mortality.
| Factor | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | CI 95% | P | HR | CI 95% | P | |
| MINO | 0.48 | 0.27–0.88 | .016 | 0.79 | 0.42–1.51 | .481 |
| Sex, female | 0.66 | 0.35–1.22 | .183 | 0.60 | 0.30–1.21 | .150 |
| Age, years | 1.06 | 1.03–1.09 | <.001 | 1.04 | 1.01–1.07 | .005 |
| Diabetes mellitus | 1.86 | 0.96–3.62 | .066 | 0.99 | 0.46–2.16 | .983 |
| Previous MI | 1.55 | 0.65–3.66 | .32 | 0.63 | 0.22–1.79 | .382 |
| PCI performed | 1.15 | 0.46–2.93 | .764 | 0.51 | 0.19–1.37 | .183 |
| Anterior MI | 2.2 | 1.20–4.03 | .011 | 0.84 | 0.43–1.67 | .626 |
| Killip >1 | 17.02 | 7.19–40.33 | <.001 | 4.45 | 3.19–6.21 | <.001 |
| GFR (MDRD), mL/min | 0.97 | 0.96–0.99 | <.001 | 0.99 | 0.97–1.00 | .283 |
| Cardiac arrest | 19.45 | 9.52–39.76 | <.001 | 5.18 | 2.29–11.73 | <.001 |
GFR, glomerular filtration rate; MI, myocardial infarction; MINO, myocardial infarction network organization; PCI, percutaneous coronary intervention.
When only the complete cases dataset was used to evaluate the effect of the MINO on the endpoint of the study, we found only subtle differences in the value of the hazard ratio: HR, 0.65 (0.31–1.36).
DiscussionAlthough our organization system to provide rapid access to reperfusion therapy to patients with STEMI is very effective at reducing time to treatment, we failed to demonstrate a significant reduction in overall mortality 30 days after the acute event.
The clinical efficacy of an organization to provide rapid access to reperfusion in patients with ST-segment elevation myocardial infarction should be evaluated since its implementation. Unfortunately, not all the patients who have an acute myocardial infarction get a rapid reperfusion therapy as they do not always use these organizational systems and, as such, this fact give the opportunity to compare the differences between both groups i.e., those who get the reperfusion therapy using an organized system and those who not.
In our study, the main findings were: a) the baseline characteristics of the population in both groups were different, with the patients who reach the hospital with the organization system having a different risk factor profile (lower prevalence of diabetes mellitus, higher glomerular filtration rate) as well as lower values when assessing TIMI Risk and CRUSADE scores; b) most of our patients were treated with primary PCI instead of on-site fibrinolysis; c) the main goal is accomplished: time to reperfusion therapy is strikingly reduced, specially the time since the arrival to the emergency room to the introduction of the guidewire in the culprit coronary artery; d) as a consequence the incidence of in-hospital heart failure is reduced; and e) a survival advantage of this system in the short-term is not demonstrated.
The organization of a system to get rapid reperfusion in the instance of STEMI is complex and requires the interplay between very different counterparts. Our system is set up as follows: a patient with symptoms suggestive of myocardial infarction can seek help in 2 different ways. First, by going by his/her own means to a nearby hospital with or without a primary PCI program. The emergency doctor in this hospital can activate the MINO to hasten the reperfusion therapy, either fibrinolysis or on-site primary PCI or urgent transfer to a PCI-capable hospital. The second approach is to make a phone call to activate MINO and get an ambulance to the nearest hospital with a primary PCI program. This type of organization is very similar to those reported in the literature and in accordance to the recommendations in current guidelines for the care of patients with acute coronary syndromes.12
We found a moderate 30-day mortality rate in both groups, with a striking numerical difference in favor of patients in the MINO group. This difference, although significant in univariable analysis, was no longer significant in multivariable models. Multiple reasons could explain this mortality rate compared with other previous studies. First, our study was conducted in “real life”, including all patients with symptoms of acute myocardial infarction given a higher mortality rate (patients with STEMI and out-of-hospital cardiac arrest were not excluded). Second, our population was relatively old, with 188 (31.6%) patients aged 75 or older, which is a higher percentage when comparing to other studies (25%). This population is usually under-represented in clinical trials and the age is a well-known factor for poor clinical outcomes in STEMI.13
In the real-world scenario, the FAST-MI 2010 registry provides a characterization of the STEMI and non-STEMI patients. They describe an increase in primary PCI and a reduction in complications rate and in-hospital mortality compared with the previous French registries.9 Cordero et al.14 also found an increased in primary PCI after the implantation of the infarct protocol in their institution as well as a major incidence of patients presenting STEMI. Our findings are in accordance with these results, since most of our patients are treated by primary PCI with a low rate of on-site fibrinolysis.
This type of organization is similar to different systems around the world that have the same goals. For example, the regional system of care demonstration project is an analysis of the protocols that have emerged across the United States to organize the regional STEMI care. This project demonstrated that emergency medical services transported-patients were different from self-transported patients in time from symptoms onset to first medical contact, incidence of cardiac arrest and in-hospital mortality. The authors also demonstrated an increase in the proportion of patients meeting the guidelines recommendations.7
Although the time from symptoms onset to primary angioplasty is reduced with the MINO, it is necessary to note that a median of 190min is a relatively long time and that this delay is difficult to reduce; Jollis et al. recently noted that this time has not changed in the last 2 decades, with a median time of 2h.7,15,16 Also the baseline characteristics of our population should be taken into account, with a high percentage of people aged 75 or older, since this group might have longer delays in seeking medical care due to several reasons, among them, the higher prevalence of atypical symptoms.15
Unfortunately, we did not split this time into shorter periods of clinical importance, and we cannot provide such interesting information. Knowledge of the time delay between symptoms onset to the first medical contact, to the first electrocardiogram and to the first definite diagnosis could be of utmost importance to implement the necessary actions to reduce delays. This effort has been evaluated by Terkelsen et al.17suggesting that the best way to accomplish a reduction in these delays would be the optimization in triaging patients in pre-hospital and in-hospital settings.
The efficacy of these systems has been evaluated analyzing the results before and after the implantation of the system. However, it would be interesting to evaluate the impact on acute myocardial infarction treatment after the implementation of such a system, since not all patients get to the hospital using these systems. This is one of the strengths of our study. Since not all patients with STEMI arrive at the hospital using the network organization, we can compare the efficacy in the “real world”, avoiding some of the biases imposed by a simpler design, a pre–post study. The results for this type of design have been consistent: a reduction in mortality with the initiation of a rapid access to reperfusion system. However, some caveats must be considered, including selection bias, historical bias, measurement bias, among others. In this regard, our study adds more information by evaluating the efficacy of our organizational system since its implementation, comparing those patients who reach the hospital by their own means and by the emergency medical services during the same period of the time, thereby avoiding the well-known biases of pre- and post-studies.
The endpoint of our study (overall mortality at 30 days) was pointedly chosen. A longer period of follow up can be of interest, but it seems likely that the effect of the MINO could be tarnished. Mid- or long-term mortality after STEMI can be related to a large number of variables, and the influence of these variables can change over time. To evaluate the real clinical impact of MINO, we decided on 30-day overall mortality as the primary endpoint, since long-term mortality can be influenced by a large number of variables, such as the presence of diabetes mellitus, renal failure, age, etc. In this regard, short-term mortality is usually assessed at 30 days, as seen in the meta-analysis by De Lucca et al.18
LimitationsThis study was not randomized and, as such, a definite conclusion about the efficacy of the MINO cannot be reached. However, it provides real-world information and the results are of importance to improve the assistance and reduce mortality.
Some non-observed variables could have influenced the results. Among them, a measure of frailty was not performed, so the influence of this factor cannot be analyzed.
It is important to highlight that this is a single-center experience with a well-defined protocol for attending STEMI. For this reason, the results reported should not be extrapolated to populations with different demographics or with different ways to provide reperfusion to STEMI. The lack of efficacy reported should be evaluated with caution, but, in our opinion, these results can help other researchers or people involved in the organization of health systems to set up a system with the highest efficacy to reduce clinical endpoints.
We calculated the sample size assuming a huge reduction of 60% of mortality at 30 days, based on the previous analysis, not considering the presence of confounders that might reduce the impact of the intervention. A larger sample size would be desirable to reduce the confidence intervals of the hazard ratios in the Cox regression models and to apply statistics tools as propensity score methods. Based on the assumptions made to calculate the sample size, a significant effect of the MINO is very unlikely.
The time elapsed since symptoms onset to the first medical contact is of utmost importance to decide the type of reperfusion treatment. Unfortunately, we do not have this information, although this variable is being appraised in a new ongoing data base, and we will continue to audit the system to detect potential points of improvement.
Finally, those patients with ST segment elevation myocardial infarction who were not reperfused were not included in our study. As such, the quantification of the overall mortality of the whole cohort of patients with this event cannot be exactly assessed.
Conclussions
In conclusion, an organized system to provide rapid reperfusion therapy to patients with acute myocardial infarction is very effective, reducing the time to reperfusion therapy. However, the impact of the system on short-term total mortality is arguable.
The benefits of early reperfusion strategies are well-established. The efficacy of the networks to provide a rapid access to these strategies has been evaluated analyzing the results before and after the implementation of these systems.
Does it contribute anything new?Our study provide information to evaluate the clinical impact after the settlement of an infarction network organization by comparing prospectively 2 groups according to the use or not of the network for a rapid reperfusion in our community, since not all patients with STEMI arrive at our hospital using such system, we could compare the efficacy in the real world, avoiding some of the biases imposed by a pre–post study.
None declared.