Heart rhythm disorders are a frequent cause of consultation for pediatric cardiologists all over the world. Arrhythmias can present congenitally in a structurally normal heart, consequence of a congenital heart defect itself or secondary to surgical or interventional correction. Radiofrequency ablation is a minimally invasive technique with high success rates. The objective was to evaluate short and long-term safety and effectiveness of radiofrequency ablation, as well as outcome-related factors in a single-center cohort of pediatric patients.
MethodsA retrospective, observational, longitudinal, historical cohort study was performed with patients who underwent radiofrequency ablation between 2001 and 2016 at our institution. We documented clinical and electrophysiological characteristics, final diagnosis, results, time of recurrence, and complications.
ResultsA total of 872 radiofrequency ablation procedures were performed between 2001 and 2016, in 762 patients, 16.9% of which had congenital heart disease. Overall success rate was 90.7%. Recurrence occurred in 16.9% of cases. The most frequent complication was atrioventricular block in 1.26%. The most common indication was accessory pathway in 69.5% of cases.
ConclusionsRadiofrequency ablation is a safe and effective treatment for arrhythmias in children because of its high rate of success, safety, and low rate of complications. The presence of congenital heart disease increases the complexity of the procedure and increases the rate of recurrence.
Las alteraciones del ritmo cardiaco son una causa frecuente de consulta para el cardiólogo pediatra en todo el mundo. Las arritmias se pueden presentar congénitamente en un corazón estructuralmente sano, como consecuencia de una cardiopatía congénita o secundaria a un procedimiento, ya sea quirúrgico o intervencionista para la corrección de una cardiopatía congénita. La ablación con radiofrecuencia es un procedimiento mínimamente invasivo con una alta tasa de éxito. El objetivo de este trabajo fue evaluar la seguridad a corto y largo plazo, así como la efectividad de la ablación con radiofrecuencia, así como los factores relacionados con el resultado en una cohorte de pacientes pediátricos en un solo centro de estudio.
MétodosSe realizó un estudio retrospectivo, observacional, longitudinal de tipo cohorte histórica en pacientes a los que se realizó ablación con radiofrecuencia entre los años 2001 y 2016 en nuestra institución. Se documentaron las características clínicas y electrofisiológicas, el diagnóstico final, el resultado del procedimiento, el tiempo de recurrencia y las complicaciones.
ResultadosSe realizaron un total de 872 ablaciones con radiofrecuencia entre los años 2001 y 2016 en 762 pacientes, 16,9% tenían una cardiopatía congénita. El éxito global del procedimiento fue del 90,7%. La recurrencia total fue del 16,9%. La complicación más frecuente fue el bloqueo auriculoventricular en el 1,26% de los casos. La indicación más frecuentre para el procedimiento fue la presencia de una vía accesoria en el 69,5% de los casos.
ConclusionesLa ablación con radiofrecuencia es un procedimiento seguro y efectivo para el tratamiento de las arritmias en niños por su alta tasa de éxito y seguridad, y su baja tasa de complicaciones. La presencia de cardiopatías congénitras aumenta la complejidad del procedimiento e incrementa la tasa de recurrencia.
Heart rhythm disorders are a frequent cause of consultation for pediatric cardiologists all over the world. Arrhythmias can present congenitally in a structurally normal heart, consequence of a congenital heart defect, or secondary to surgical or interventional correction. Disorders in heart rhythm can present from fetal life until adulthood. They present in approximately 5% of pediatric patients, mainly in infants, preschoolers, and adolescents.1,2 The most frequent arrhythmia is supraventricular tachycardia, in about 1 of 250 children. It can be divided into 3 groups: reentry with an accessory pathway, reentry without an accessory pathway, and ectopic tachycardia. In patients with a structurally normal heart, about 75% to 90% of all supraventricular tachycardia correspond to an accessory pathway3–6 and most of them are concealed, atrioventricular (AV) nodal reentry represents approximately 15% of all supraventricular tachycardias.7,8 Atrial flutter and atrial fibrillation are rare in this group of patients but become more frequent in those who have undergone a surgical procedure.
In pediatric patients, a very important group to consider are those with a congenital heart defect, since 5% to 35% of these patients have a concomitant heart rhythm disorder. The main congenital heart defects associated with arrhythmias are atrial septal defect, ventricular septal defect, atrioventricular septal defect, tetralogy of Fallot, Ebstein's anomaly, transposition of great arteries, congenitally corrected transposition of great arteries, and cardiac rhabdomyomas in patients with tuberous sclerosis, which is associated to Wolff-Parkinson-White syndrome.9–12 The surgical correction of these heart defects is also associated with heart rhythm disorders since scars confer an anatomical substrate for macro re-entry circuits.
Radiofrequency ablation has proven to be a safe an effective treatment, because of its high rate of success, low rate of complications, and low rate of recurrence13-16. Among infants younger than 1 year of age, supraventricular tachycardia frequently resolves spontaneously, which is why it is preferable to wait until after 5 years of age.17-19
Techniques like 3D electroanatomical mapping allow to conjoin anatomical with electrophysiological information to enhance localization of the arrhythmogenic site and to improve the effectiveness of the procedure.20–22 This is very important, particularly in patients with very complex arrhythmias, congenital heart defects, antecedent of surgical procedure, and those with recurrence after a previous ablation. It also has the benefit of a reduction of procedure time, which is relevant in our group of study because of the need for sedation and anesthesia, and the exposure to radiation in pediatric patients and medical staff.
Radiofrequency ablation has been compared to cryoablation, especially in pediatric patients, and cryoablation indeed reduces the fluoroscopy exposure and complications,17,23 but it is also true that this technique has a higher rate of recurrence, reported in up to 45% of cases, concluding that it has no statistically significant superiority in pediatric patients.6,24–27
It is important to define the experience of our institution in the treatment of arrhythmias with radiofrequency ablation since it has a huge impact on the quality of life of patients with heart rhythm disorders.
The objective was to evaluate short- and long-term safety and effectiveness of radiofrequency ablation, as well as factors related to outcomes in a 15-year study of a cohort of pediatric patients from a single-center.
MethodsAn observational, longitudinal, and retrospective historical cohort study was performed with patients who underwent radiofrequency ablation between 2001 and 2016 at our institution.
A procedure record dataset was built with data of all radiofrequency ablation procedures performed in patients 18 years of age or younger, between 2001 and 2016. We documented clinical and electrophysiological characteristics, final diagnosis, results, time of recurrence, and complications. All patients were followed-up as protocol at our institution every 6 months for the first year after the ablation and then every year since then. Follow-up consisted in physical examination, electrocardiogram (ECG), and 24-h Holter when attending physician considered necessary. Recurrence of arrhythmias was defined as a new onset tachycardia documented on follow-up ECG, Holter monitor, or ECG during tachycardia in an emergency room visit due to symptoms. Every patient was recommended to immediately contact our institution in case of new-onset arrhythmia symptoms for an emergency consultation.
We included male or female patients with age from 1 day of extrauterine life up to 18 years old; since in our institution this is the age group of pediatric patients; who underwent radiofrequency ablation, with confirmed diagnosis during the electrophysiological study. We excluded all patients with heart rhythm disorders that did not require radiofrequency ablation and all cryoablation procedures since the experience in pediatric patients with this technique in our institution during the period of this study is too limited. We also excluded patients who no longer have follow-up records at our institution.
Our outcomes were a success in the procedure, defined as the specific electrophysiologic criteria for each type of arrhythmia; complications during the same hospitalization, and the first-month post-ablation and recurrence of the arrhythmia defined as a new onset tachycardia documented during the follow-up.
Statistical analysisThe descriptive analysis was based on the elaboration of summary, central tendency, and dispersion measures. For statistical analysis, discrete and continuous quantitative variables and qualitative nominal and ordinal were defined. Nominal and ordinal variables were described according to their frequency, and quantitative with summary measures based on their distribution as mean and standard deviation. For the evaluation of the distribution of continuous quantitative variables, the Kolmogroff–Smirnoff test was used. Logistic regression analysis was performed to assess the likelihood of recurrence based on patient characteristics, risk of recurrence was represented in terms of odds ratio, and percentage reduction of risk using logit evaluation. For the elaboration of the analysis two commercial software packages were used: SPSS for MAC version 20 and STATA for windows version 13.1
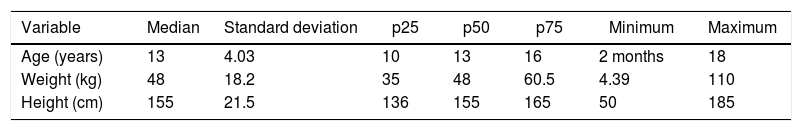
ResultsBetween 2001 and 2016, a total of 872 radiofrequency ablation procedures, in 762 patients, were performed at our institution. Of these procedures, 59% (n=518) were performed in male patients, while 41% (n=354) in female patients. The median age was 13 years, with a minimum of 2 months of age. The median of weight was 48kg, with a standard deviation of ±18.2kg. Patients characteristics are summarized in Table 1.
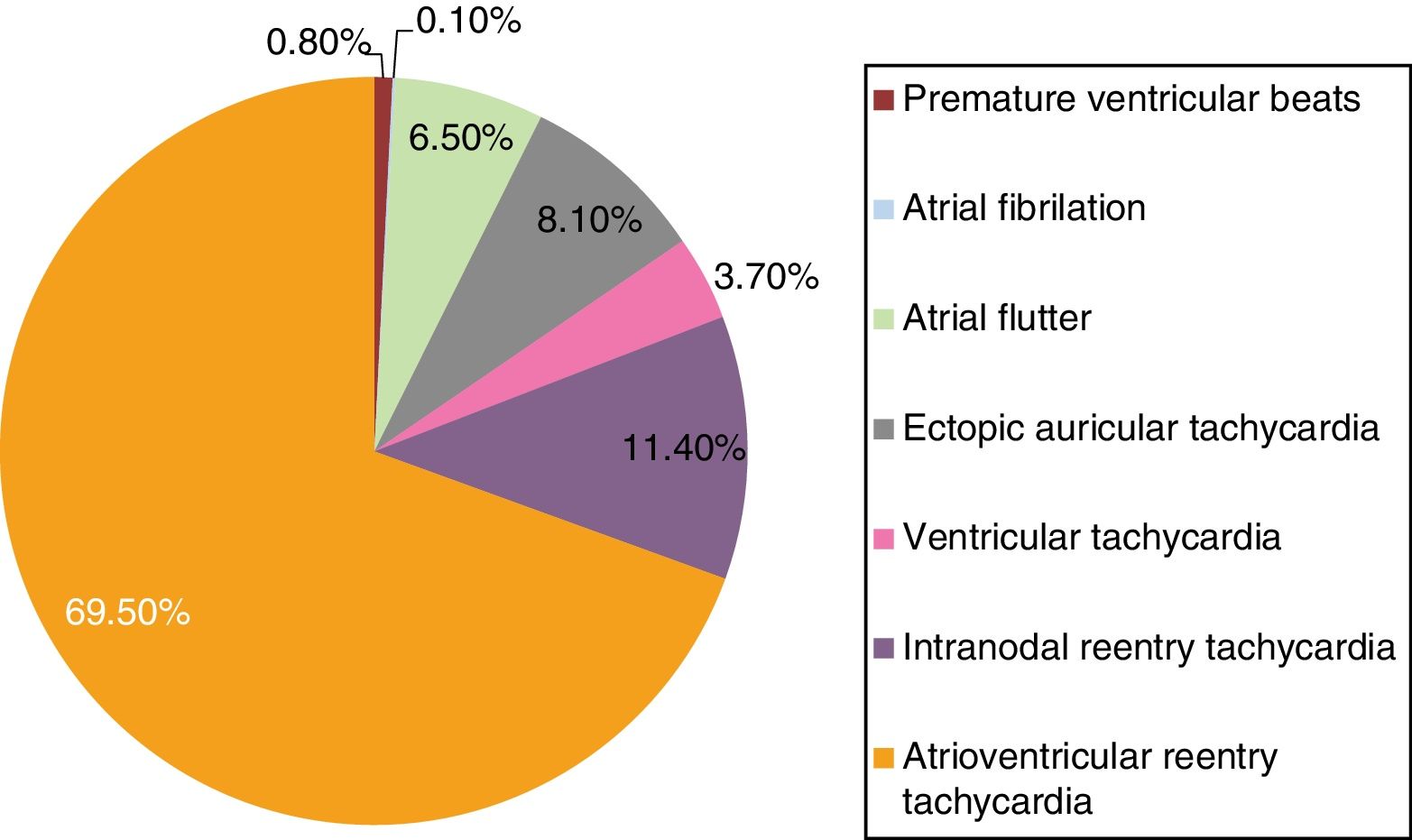
All patients reported symptoms, mainly palpitations. Episodes of supraventricular tachycardia were documented on electrocardiogram or Holter monitor before the procedure only in 47% (n=410) of patients, the remaining patients (53%) the indication for procedure was either manifest preexcitation on resting ECG or high burden of symptoms. The most frequent final diagnosis was accessory pathway in 69.5% of patients (n=606), distribution of diagnosis is summarized in Fig. 1.
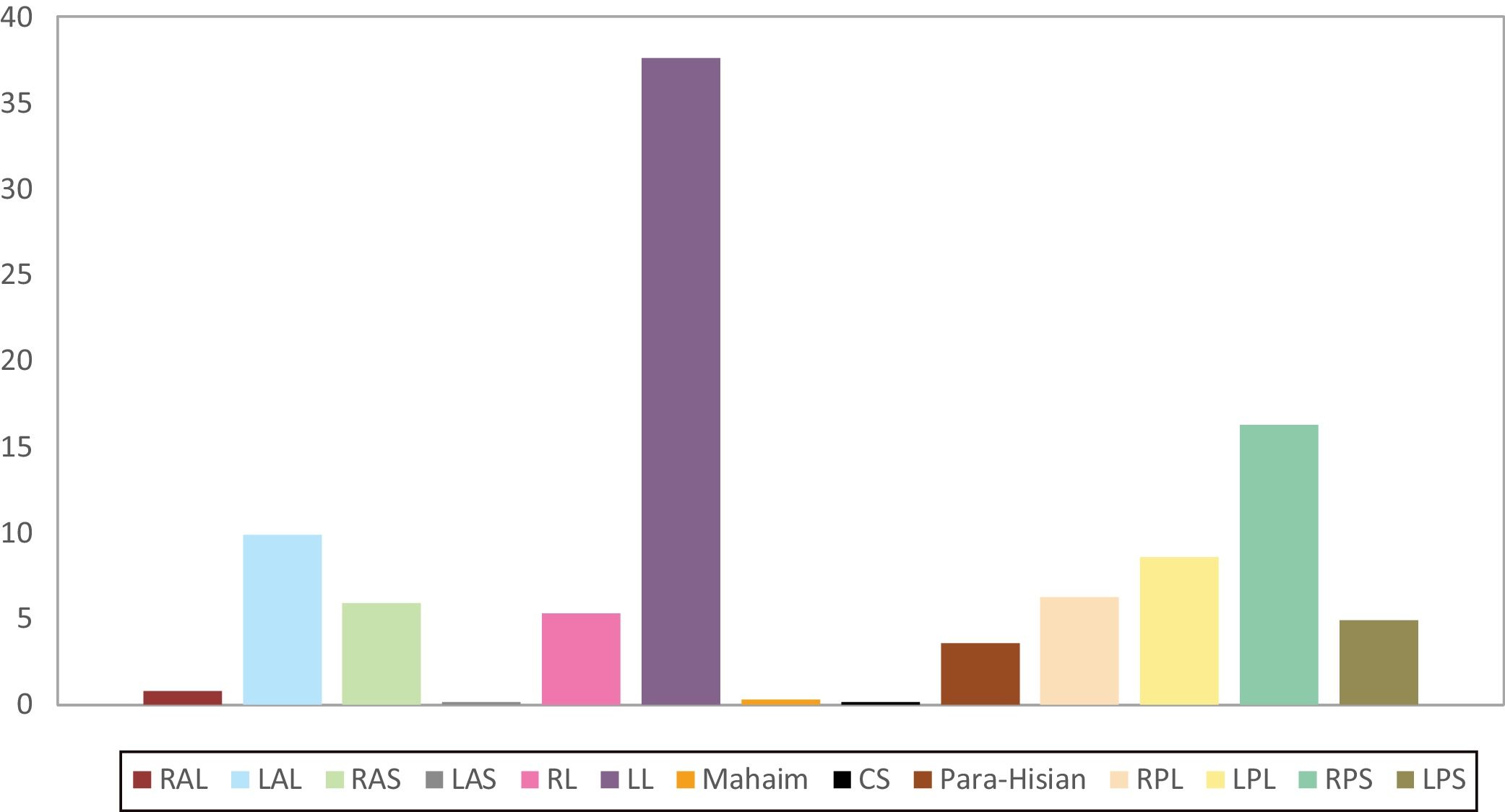
In patients with a diagnosis of atrioventricular reentry, 71.8% (n=435) had a manifest accessory pathway and the rest, 28.2% (n=171) had a concealed accessory pathway. Specific localization of accessory pathway is summarized in Fig. 2.
Localization of accessory pathways. CS, coronary sinus; LAL, left anterolateral; LAS, left anteroseptal; LL, left lateral; LPL, left posterolateral; LPS, left posteroseptal; RAL, right anterolateral; RAS, right anteroseptal; RL, right lateral; RPL, right posterolateral; RPS, right posteroseptal.
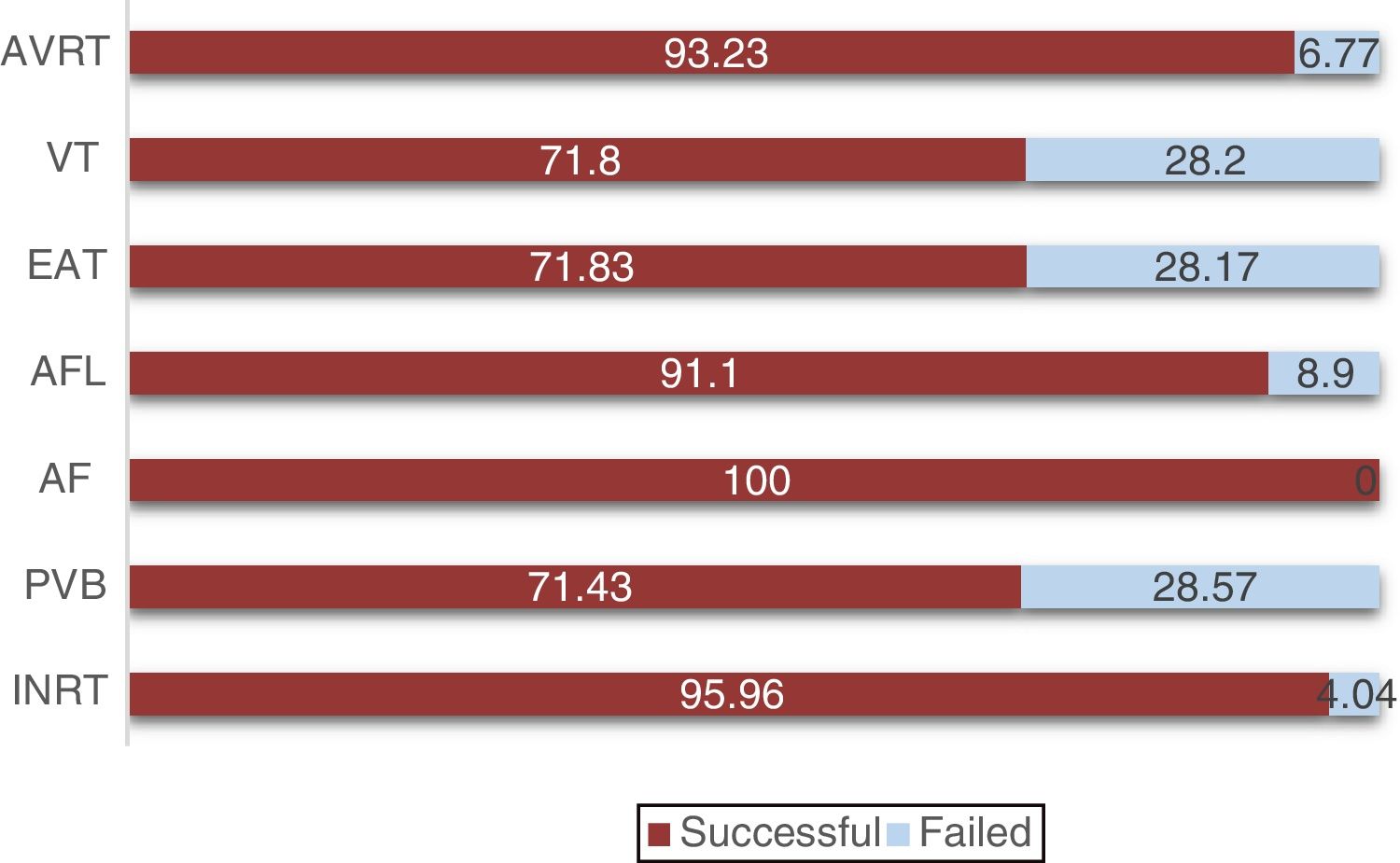
The overall global success was reported in 90.7% (n=791) and failure in 9.3% (n=81). In patients with AV nodal reentry, the procedure was successful in 96% (n=95) and failed in 4% (n=4), in patients with premature ventricular beats, it was successful in 71.4% (n=5), and failed in 28.5% (n=2), in atrial flutter, it was successful in 91.1% (n=51), and failed in 8.9% (n=5), in ectopic atrial tachycardia it was successful in 71.8% (n=51), and failed in 28.2% (n=20), in ventricular tachycardia it was successful in 71.8% (n=23), and failed in 28.2% (n=9), in atrioventricular reentry it was successful in 93.2% (n=565), and failed in 6.8% (n=41) (Fig. 3).
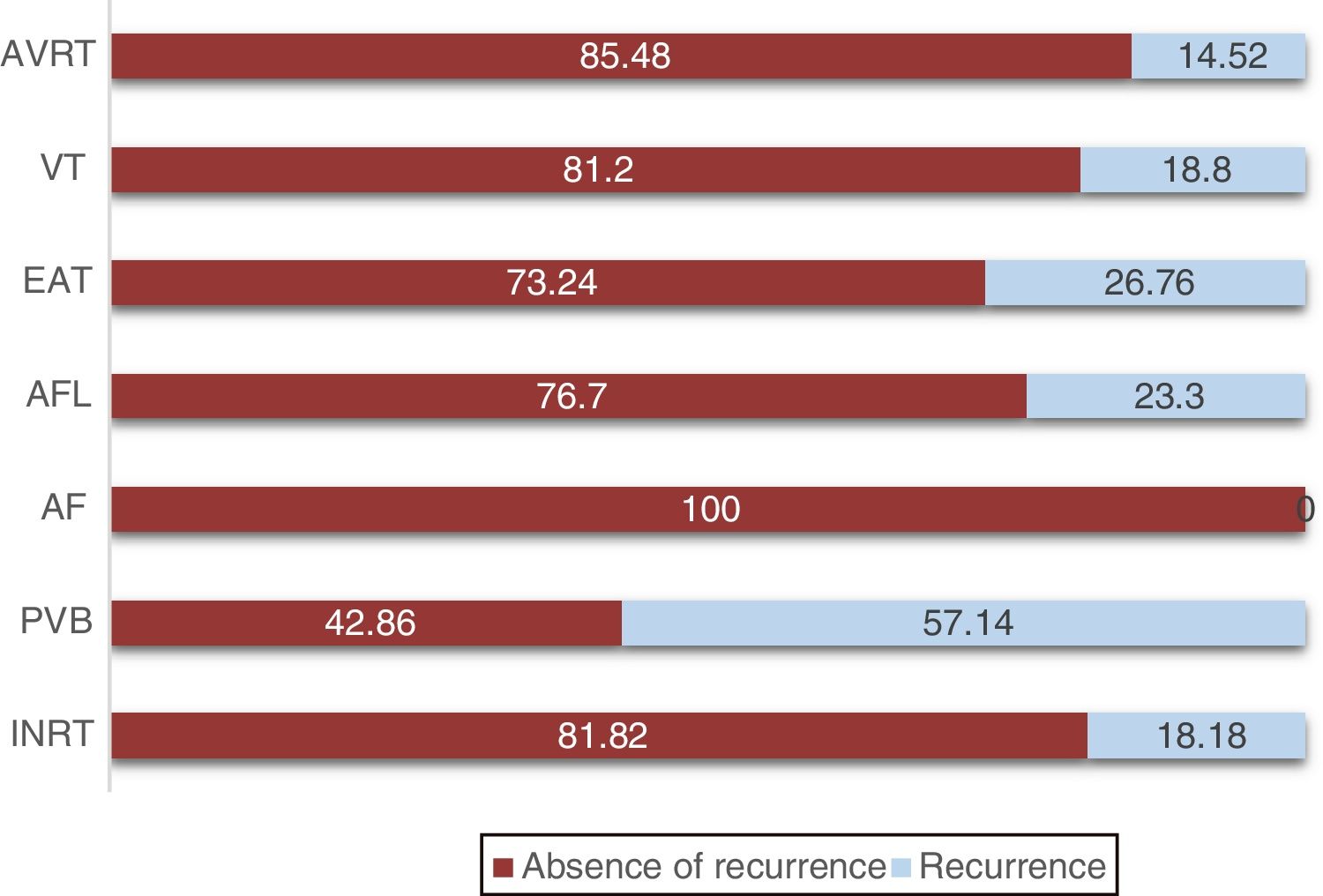
Recurrence of arrhythmia was reported in 16.9% (n=148) of all procedures. According to the type of heart rhythm disorder, it was reported in 18.2% (n=18) of the patients with AV nodal reentry, in 57.1% (n=4) of patients with premature ventricular beats, in 23.3% (n=13) of patients with atrial flutter, in 26.7% (n=19) of patients with ectopic atrial tachycardia, in 18.8% (n=6) of patients with ventricular tachycardia and in 14.5% (n=88) of patients with atrioventricular reentry tachycardia (Fig. 4). Mean recurrence time for patients with AV nodal reentry was of 16.7 months, for premature ventricular beats of 4.5 months, for atrial flutter of 24.9 months, for ectopic atrial tachycardia of 6.9 months, for ventricular tachycardia of 32.7 months, and for atrioventricular reentry of 8.6 months.
Regarding procedure technique, radiofrequency ablation is related to relatively high fluoroscopy time. In this cohort, we found a median duration of fluoroscopy of 17min, (minimum of 2 and a maximum of 90min). The procedure that required more fluoroscopy time were ventricular tachycardia ablation, with a mean of 26.6min±15.7min, followed by atrial flutter with a mean of 22.8min±10.4min, accessory pathway with a mean of 21min±16.5min, premature ventricular beats with mean of 15.6min±3.2min and AV nodal reentry with mean of 13.7min±7.6min.
Complications were reported in 2.7% of all cases. The most frequent complication was auriculoventricular block in 1.26% of all procedures (n=11), requiring the placement of a pacemaker in 36.3% of these patients (n=4). Other complications were steam pop (0.23%, n=2), femoral venous thrombosis (0.23%, n=2), acute arterial thrombosis (0.11%, n=1), superior vena cava syndrome (0.11%, n=1), severe vasovagal reaction (0.11%, n=1), atrial paralysis or standstill (0.11%, n=1) which is a rare condition characterized by the absence of electrical and mechanical activity in the atria, hematoma at the puncture site (0.11%, n=1), retroperitoneal hematoma (0.11%, n=1).
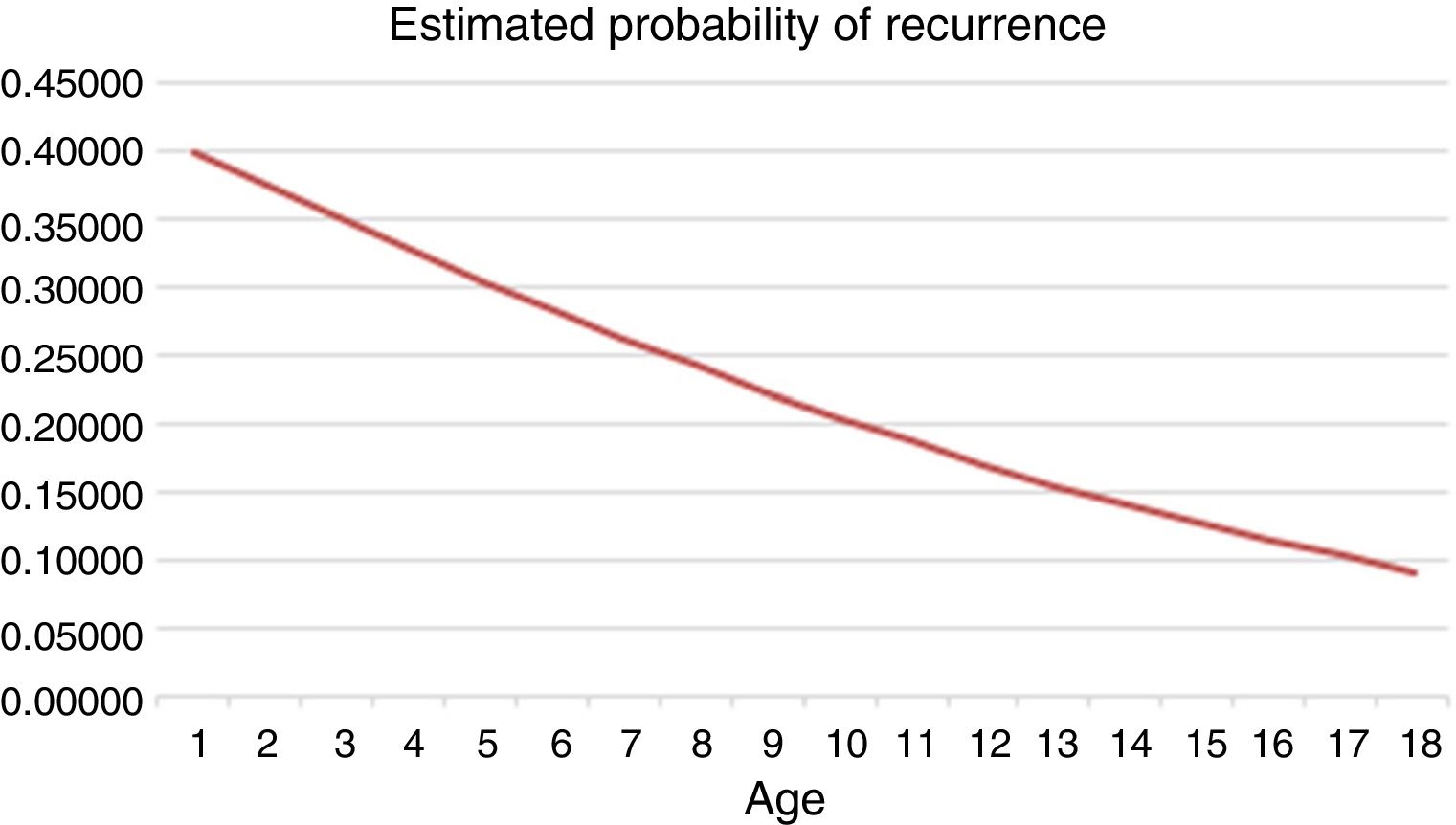
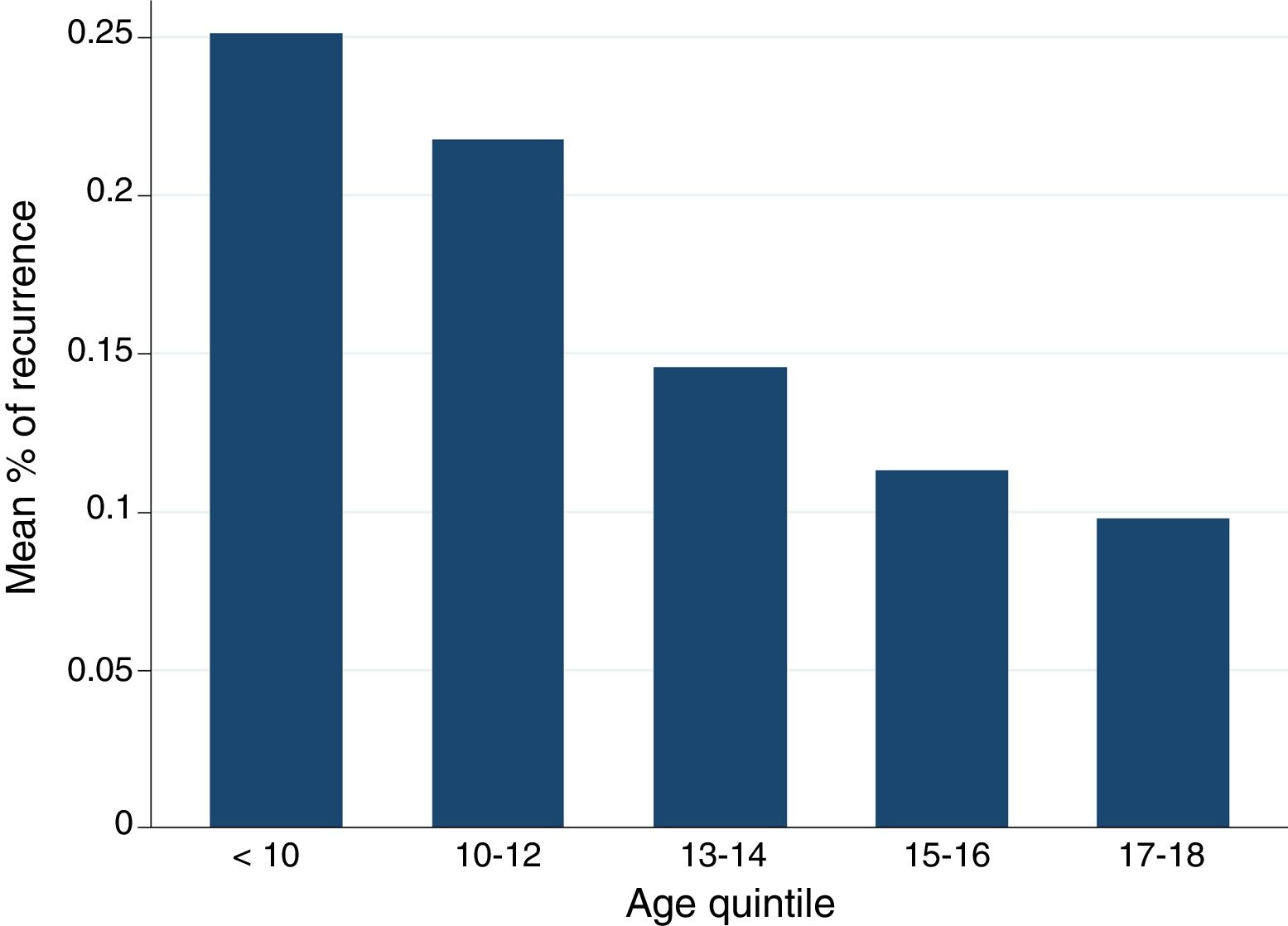
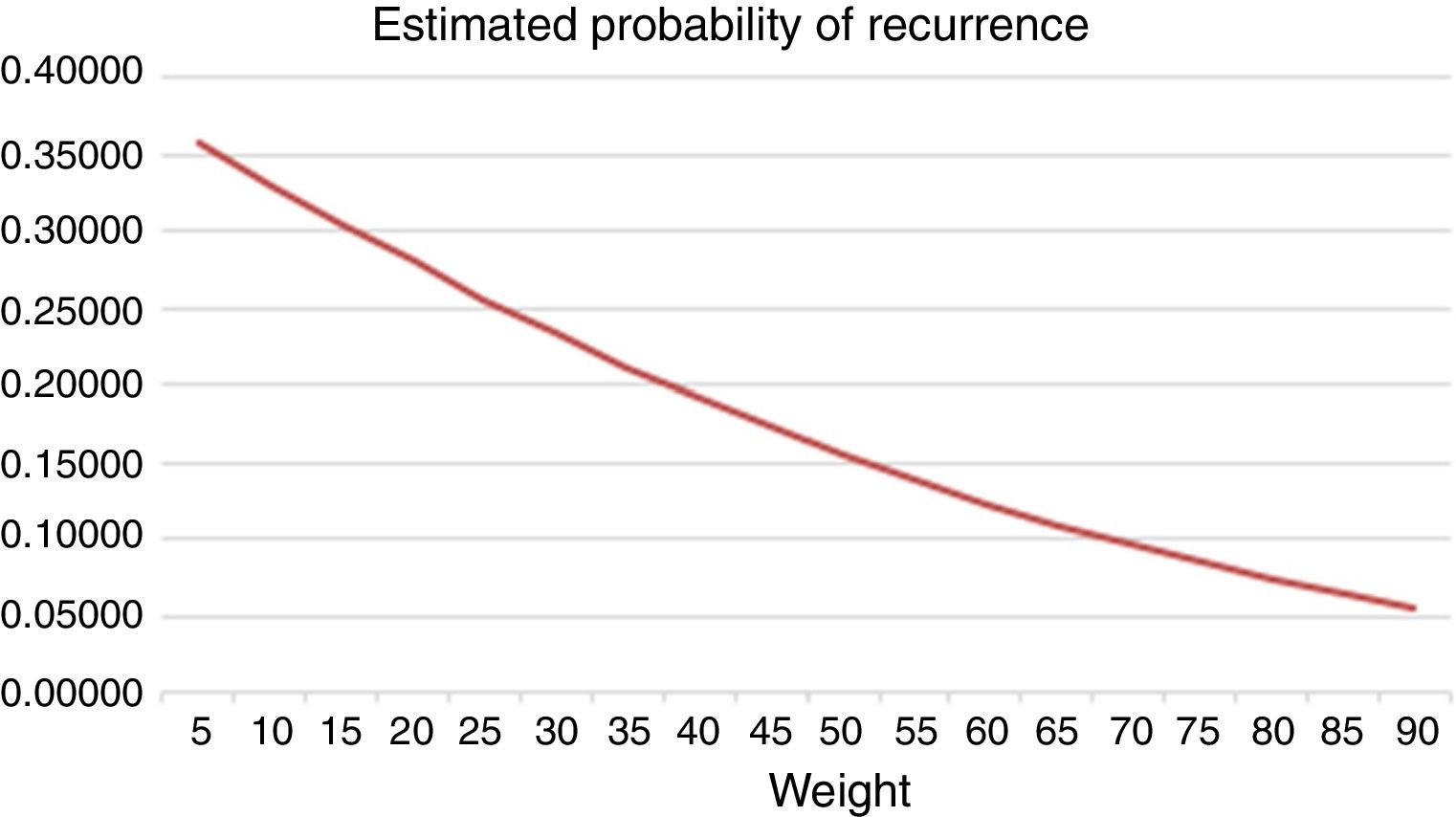
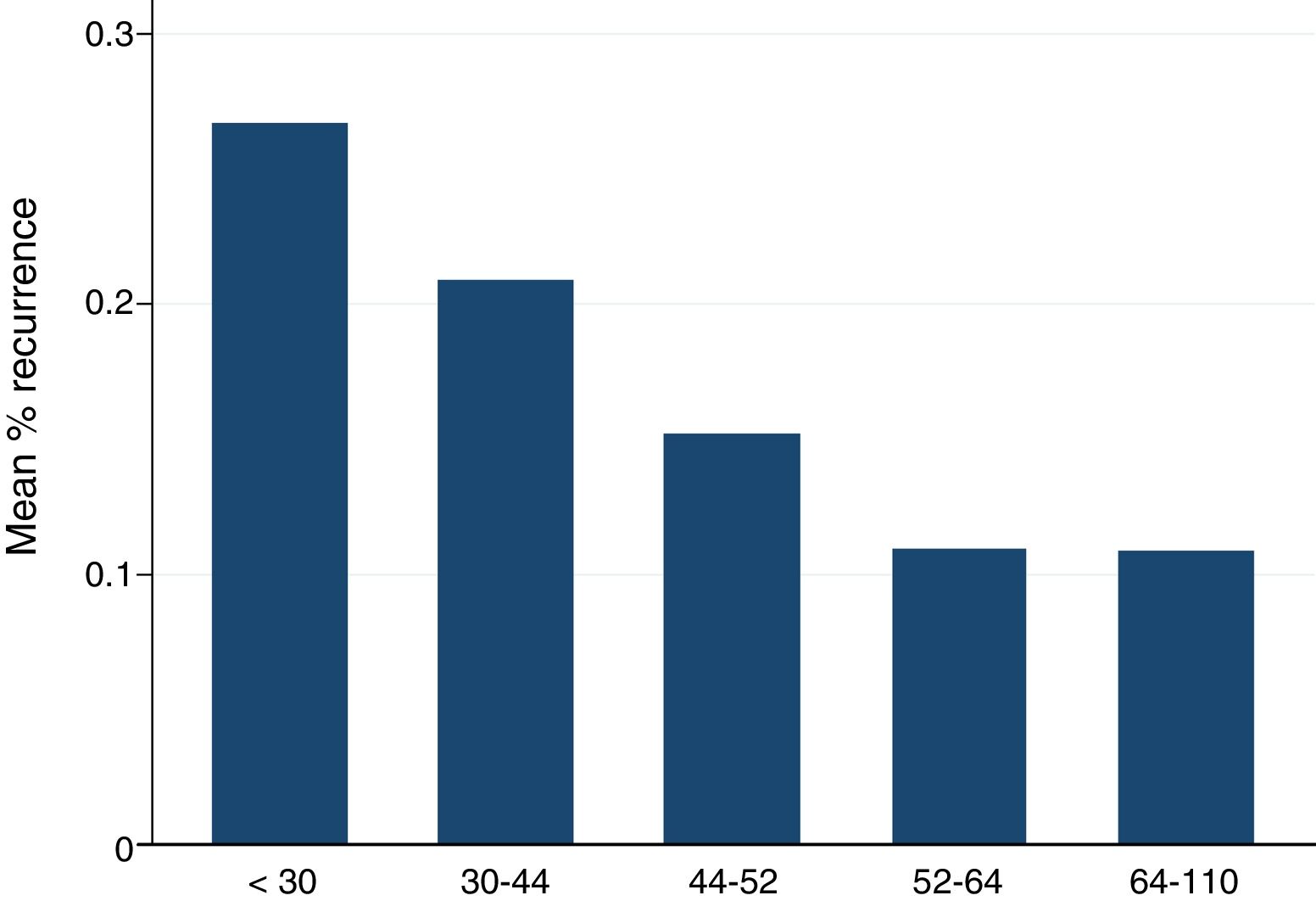
Factors related to the risk of recurrence were studied. In an overall analysis, including every type of ablation, age, and weight were the only factors that correlate statistically significant with recurrence risk. Using linear regression model, we found that age had an impact in recurrence (odds ratio[OR], 0.89; 95% confidence interval [95%CI], 0.85–0.93; P<.001), with an important reduction as age increases (Fig. 5). Patients older than 12 years of age had a reduction of 10% of recurrence risk. We divided patients in quintiles, the ones younger than 10 years old had a mean percentage or recurrence of 25%, the ones between 10 and 12 years of age had a mean percentage of recurrence of 22%, the ones between 13 and 14 years of age had a mean percentage of recurrence of 14%, the ones between 15 and 16 years of age had a mean percentage of recurrence of 11% and the ones older than 17 years of age had a mean percentage of recurrence of 9% (Fig. 6). According to sub-analyses regarding type of procedure, age had an impact in recurrence risk especially in accessory pathway ablation (OR, 0.87; 95%CI, 0.82–0.92; P<.001) and atrial flutter ablation (OR, 0.80; 95%CI, 0.68–0.94; P<.01). According to the logistic regression model, weight was also a good predictor of recurrence (OR, 0.97; 95%CI, 0.96–0.98; P<.001). In those patients with bodyweight above the mean value (48kg) the risk of recurrence was significantly lower than in patients with body weight below 48kg (Fig. 7). After the division of patients in quintiles according to weight, we found that patients in the upper 3 quintiles (> 44.5kg) had lower recurrence risk than patients with less body weight, with up to 15% risk reduction in patients in the 5th quintile (> 64kg) (Fig. 8). Specific type of procedure sub-analyses found that weight was especially important predictor factor for recurrence in atrial flutter (OR, 0.94; 95%CI, 0.90–0.98; P<.01) and accessory pathway ablation (OR, 0.96; 95%CI, 0.95–0.98; P<.001).
Of all patients, 16.9% had a structural heart defect, the most frequent were: Ebstein anomaly, dilated cardiomyopathy, total anomalous pulmonary venous connection, and atrial septal defect. In patients with Ebstein anomaly, the 87.5% (n=42) of cases the ablation procedures were successful, 50% of ablations in patients with transposition of great arteries were successful, 63.1% of procedures in patients with dilated cardiomyopathy were successful; 50% of the ablations in patients with pulmonary atresia with ventricular septal defect were successful, 100% of procedures in patients with tricuspid atresia with pulmonary stenosis were successful, 88.2% were successful in patients with total anomalous pulmonary venous connection; 94.1% were successful in patients with atrial and ventricular septal defect, 100% were successful in patients with aortic coarctation, double outlet right ventricular, situs inversus with dextrocardia, pulmonary stenosis, patent ductus arteriosus, tetralogy of Fallot, bicuspid aortic valve, double inlet left ventricular, double mitral orifice, left ventricular noncompaction, hypertrophic cardiomyopathy, atrial myxoma, truncus arteriosus.
During the time frame of this study electroanatomical mapping was not available until 2010, since then CARTO or ENSITE systems, were used in 8.6% of the procedures, of this, 85.3% (n=64) was successful. The recurrence of this procedure was 30.7% (n=23).
DiscussionIn the last 15 years, our institution has achieved great and valuable experience in radiofrequency ablation, with a very high rate of success and low rate of complications. Wolff-Parkinson-White syndrome is the first indication for electrophysiological study and ablation in this population. The rate of success and recurrence reported in our study is similar to the ones reported in international multicentric studies.14–16 The highest success rate was observed in patients with atrioventricular reentry tachycardia, and also, the lower recurrence rate. This is explained in part because of the growing expertise in this type of procedure, which is also the most common in this group of patients and with great experience in our center. This fact emphasizes the importance of experience and volume of cases to improve results in every electrophysiology laboratory.
International evidence demonstrates that bodyweight above 15kg is a strong predictor of a lower rate of complications and recurrence. In our cohort, the rate of complications was so low that a statistical analysis could not be made based on this data. Nonetheless, the risk of recurrence was suitable for analysis. We identified a significantly higher body weight as a predictor of lower risk of recurrence, in comparison with previously reported data. This could be explained by the fact that our population is older and thus heavier. We also have less experience in infants and preschooler patients.
A very important observation is that most of recurrences were after the first month of the ablation, and a lot were after the first year of the procedure, suggesting that the follow-up of those patients should be at least for a year or even longer.
Congenital heart defects are very frequent, and in our group of patients they represented 16.9% (n=147) of all the patients. The presence of a heart defect makes evident the increase in complexity of the procedure, which has a direct impact on the rate of success, the recurrence, complications, and duration of fluoroscopy. The use of electroanatomical mapping allows us to increase the success rate, despite the anatomical complexity. Electroanatomical mapping, with CARTO or ENSITE systems, in our institution was used according to the judgment electrophysiologist in charge of the ablation, and we have a low percentage of procedures supported by this technology because in the first years we did not have this technology available. Also, an important limiting factor in our center is the economic burden of this technology.
In terms of safety, we consider radiofrequency ablation as one of the most reliable procedures in pediatric interventional cardiology, since we had a very low rate of complications, and none of that compromised function or life of patients, considering that an important number of procedures were performed in patients with age and weight under the international mean of age and weight for treatment.
An important consideration in pediatric patients is exposure to fluoroscopy during the procedure, which is reported in our study with a median of 17min, a very acceptable time for this group of patients, considering the challenge that represents this intervention in pediatric patients because of age, weight and anatomical complexity.
ConclusionsRadiofrequency ablation is a safe and effective treatment for arrhythmias in children due to its high rate of procedure success and low proportion of complications. There are several factors that can influence the outcome of this method, particularly in terms of success rate and recurrence. Two of the most important factors are body weight and the presence of a congenital heart disease. We identified higher body weight (> 44kg) as a significant predictor of lower risk of recurrence. In the case of congenital heart disease patients, it is clear that the proportional increment in procedure complexity correlates with an increase in recurrence rate. However, the use of 3D electroanatomical mapping can help to improve the effectiveness of the procedure, particularly in this setting, with a clear impact particularly in lower recurrence rate. In light of this result, it is reasonable to recommend 3D electroanatomic mapping as a routine technique in every congenital heart disease patient.
It is known that heart rhythm disorders are very frequent among pediatric population, and effective treatment can have an important impact on the patient's life quality. Radiofrequency ablation has demonstrated to be effective and safe among this group of patients, with a very low rate of complications. To ensure the safety of the procedure it is mostly indicated in patients older than 5 years of age and weighing over 15kg.
Does it contribute anything new?In our study we demonstrated not only that weight has a major impact on the safety and success rate of the procedure, but also that the presence of congenital heart desease is determinant for the patients’ outcome. We would recommend pediatric patients have a long follow-up after the procedure, since we found that most recurrences happened a month after the ablation, and many happened after the first year.
None.
Conflicts of interestThere are no conflicts of interest.