The advantages of sedation in patients undergoing transesophageal echocardiography (TEE) are well established, but the increasing number of TEE studies may limit the capacity of anesthesiology services. In this study we analyze the effectiveness and safety of a moderate sedation program carried out by non-anesthesiology professionals (NAP).
MethodsDescriptive and prospective study that included all consecutive patients undergoing a TEE procedure under moderate sedation by NAP and by anesthesiology professionals (AP) from September 2018 to September 2019. Patients were selected according to a specific algorithm agreed upon with the Anesthesiology Department. We analyze current indications for TEE, complication rates, and recovery times associated with sedation.
ResultsWe performed 267 procedures in 252 patients (54% male, 69 years). Main indications were screening or monitoring of surgical and percutaneous cardiac interventions (47.9%), endocarditis (28.5%) and stroke (20.6%). Patients in the NAP group were younger (59 vs 71 years), less hypertensive (43% vs 61%), with less lung disease (4% vs 24%), lower risk of difficult airway (1% vs 22%) and lower comorbidity (ASA scale≥III 13% vs 77%). Complications were more frequent in the AP group (26% vs 9%), mainly mild respiratory (19% vs 9%). Events were associated with the presence of lung disease and higher ASA degree. Recovery time was longer in the AP sedation group (20min vs 15min).
ConclusionsTEE indications are changing and involve larger and more complex studies. Moderate sedation with propofol performed by NAP is safe in selected patients, with adequate recovery times.
Las ventajas de la sedación en la ecocardiografía transesofágica (ETE) están bien establecidas, pero el número creciente de estudios de ETE limita la capacidad de los servicios de anestesiología. Analizamos la efectividad y la seguridad de un programa de sedación moderada a cargo de profesionales no anestesiólogos (PNA).
MétodosEstudio descriptivo y prospectivo de pacientes consecutivos sometidos a ETE con sedación moderada por PNA y por anestesiología (PA) entre septiembre de 2018 y septiembre de 2019. Los pacientes fueron seleccionados con un algoritmo específico acordado con el Servicio de Anestesiología. Analizamos las indicaciones actuales de ETE, las tasas de complicaciones y los tiempos de recuperación asociados a la sedación.
ResultadosRealizamos 267 procedimientos a 252 pacientes (54% hombres, 69años). Las principales indicaciones fueron cribado o seguimiento de intervencionismo cardiaco estructural percutáneo o quirúrgico (47,9%), endocarditis (28,5%) e ictus (20,6%). Los pacientes del grupo PNA fueron más jóvenes (59 frente a 71años), menos hipertensos (43% frente al 61%), con menor neumopatía (4% frente al 24%), menor riesgo de vía aérea difícil (1% frente al 22%) y menor comorbilidad (escala ASA ≥III 13% frente al 77%). Las complicaciones fueron mayores en el grupo PA (26% frente al 9%), principalmente respiratorias leves. Los eventos se asociaron con la presencia de neumopatía y mayores grados de ASA. El tiempo de recuperación fue significativamente mayor en el grupo PA (20min frente a 15min).
ConclusionesLas indicaciones de ETE están cambiando y comportan estudios de mayor duración y complejidad. La sedación moderada con propofol realizado por PNA es segura en pacientes seleccionados, con tiempos de recuperación adecuados.
Transesophageal echocardiography (TEE) is an essential diagnostic procedure in cardiology with a low complication rate in the adult population.1 However, the poor tolerance of the procedure in non-sedated patients made it necessary to carry out studies that were very focused on the pathology being sought, especially when the indications were sources of systemic embolism and suspected endocarditis.2,3 In the last decade, the clinical profile of patients and the complexity of procedures seem to have changed. The demand for TEE studies has increased in parallel to the rise of interventional percutaneous procedures in Cardiology, usually applied in elderly patients with high comorbidity.
Moderate sedation during TEE provides comfort and amnesia from the procedure and should be available to all patients. This level of sedation also improves the quality of the studies: by creating a state of calm and cooperation, more complex and detailed examinations can be performed.
Midazolam4 and propofol5 are generally used for sedation in these procedures, being the depressant effects on the cardiovascular and respiratory systems the main concern regarding patient safety. Usually, this sedation requires the collaboration of anesthesiologists, familiar with the management of these drugs and their potential adverse effects.
The growing requirement for sedation in outpatient procedures may exceed the capacity of anesthesiology services, which has led to new approaches in which sedation is performed by non-anesthesiologist professionals (NAP) specifically trained for this purpose. Different Anesthesiology Societies, aware of this situation, have developed specific recommendations to regulate the training and adequate facilities to carry out NAP sedation.6–8 Our center has developed a pilot program of training and support in sedation with propofol administered by NAP. The objective of this work is to analyze the implementation and safety of this program in patients undergoing TEE.
MethodsInclusion criteriaWe conducted a descriptive, prospective, non-randomized and single-center study of consecutive patients undergoing TEE in our Cardiac Imaging Unit from September 2018 to September 2019. All patients were aged>18 years and signed the informed consents. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study protocol was accepted as a protocol assistance in the Quality Care Program of our hospital, and has not required approval by the Ethics Committee.
Non-anesthesiologist staff training programPrior to its start, an analysis of the workspace and the necessary material to carry out the program was made. Following international guidelines for procedural sedation and analgesia in adults,8 the training focused on:
- 1.
Assessment of the airway and comorbidities that could affect sedation.
- 2.
Competence in recognizing the different levels of sedation.
- 3.
Knowledge of the most commonly used drugs in sedation and advanced life support training with special focus on advanced airway management.
- 4.
Competence in recognizing total recovery of consciousness required to leave the monitoring area.
Finally, practical skills were acquired through supervised live cases. Training program lasted for 1 week.
Study variablesThe baseline characteristics of the patients and the presence of a priori pathologies associated with events during sedation, such as underlying lung disease (asthma, chronic obstructive pulmonary disease or sleep-apnea) or severe valvular disease were recorded. Adverse events throughout the sedation procedure until recovery were recorded on a sedation form. These events were classified as respiratory (pulse oximetry oxygen saturation<90%, need for endotracheal intubation [EI]), hemodynamic (hypotension<90mmHg, need for cardiopulmonary resuscitation), arrhythmic (bradycardia<40bpm or sustained new tachyarrhythmia), digestive (non-self-limited digestive bleeding) and neurological events (new-onset focal neurological deficits). The monitoring of the procedure and its complications were recorded in a sedation in TEE register for publication in the patient's medical history.
Study protocolWith the objective of planning sedation, this program designed a decision-making algorithm to perform a pre-anesthetic evaluation. AP sedation was performed if any of the following criteria was present. Otherwise, sedation was performed by NAP:
- -
Age>70 years-old
- -
Morbid obesity with BMI>40kg/m2
- -
Left ventricle ejection fraction<30%
- -
Chronic liver disease Child C
- -
Complex studies in American Society of Anesthesiology Physical Status Classification (ASA) III or ASA IV
- -
Chronic lung disease (sleep-apnea, chronic obstructive pulmonary disease or asthma)
- -
Chronic kidney disease with estimated glomerular filtration rate<30ml/min
For the sedation procedure the use of propofol was prioritized. The target was to keep patients in a moderate degree of sedation, also called conscious sedation, which enables spontaneous ventilation with preserved cardiovascular function.9 In all cases of NAP sedation an anesthesiologist was previously informed and available to provide support or switch to AP sedation if needed.
After the TEE, patients were transferred to a recovery area. The modified Aldrete10 post-anesthetic recovery score was used to authorize discharge, considering a score>9/10 points in hospitalized patients and>17/18 points in outpatients to finish the procedure. The time to reach the adequate Aldrete score was recorded as recovery time.
Statistical analysisCategorical variables are expressed as absolute frequencies and percentages. Quantitative variables are expressed as mean±interquartile range [IQR, 25–75%]. Quantitative variables distribution assessed using the Shapiro–Wilk test showed a significant violation of normality assumption. To compare variables between the 2 groups, Chi-square and Fisher test were performed for categorical variables and Wilcoxon test for quantitative variables.
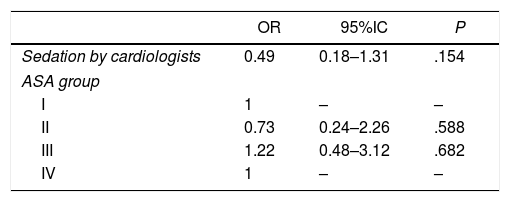
A logistic regression model was performed to explain the independent association between events, sedation group and ASA grade. Selected multivariate model had moderate discrimination (area under the curve 0.62) and moderate calibration (P value for the Hosmer–Lemsehow test=.12). The results are expressed as odds ratios (OR), with their 95% confidence intervals (95%CI). In all hypothesis tests, the null hypothesis was rejected with a type I error or alpha error < 0.05. Stata 12.1 software was used for all analysis.
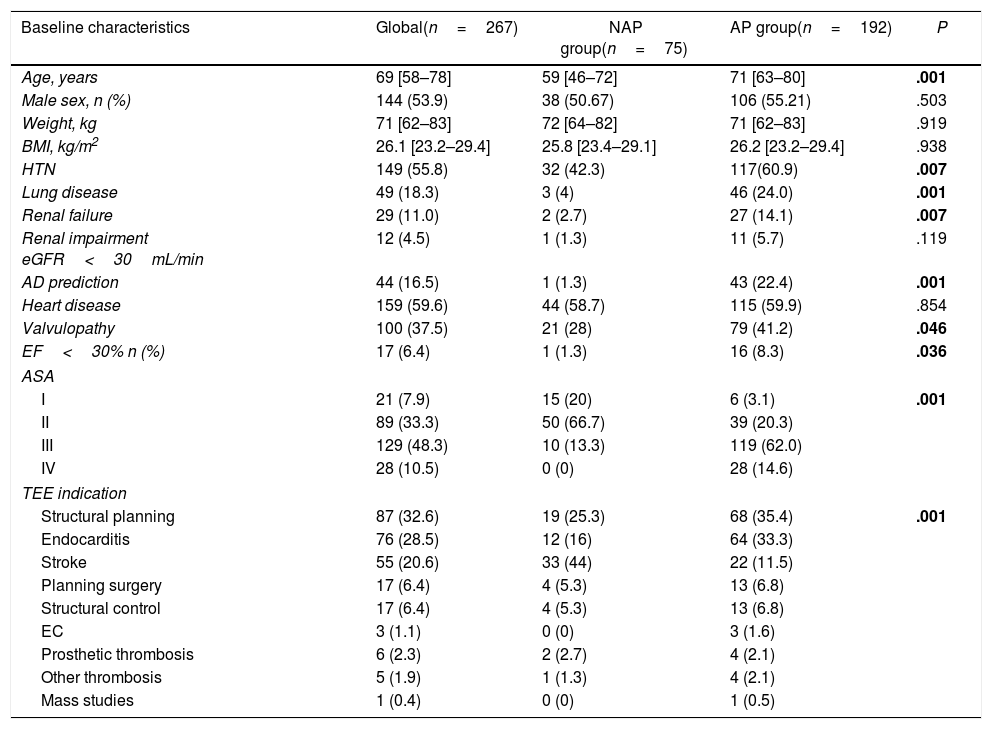
ResultsBetween September 2018 and September 2019, a total of 267 TEE were performed under sedation in 252 patients (Table 1). 54% were men and median age was 69 years. Main indications were percutaneous or surgical intervention (45.3%), endocarditis screening (28.5%) and stroke study (20.6%). Repeated TEE were mainly performed in endocarditis monitoring (55.2%), planning and follow up of structural procedures (31%) and thrombosis (10.3%).
Baseline characteristics.
| Baseline characteristics | Global(n=267) | NAP group(n=75) | AP group(n=192) | P |
|---|---|---|---|---|
| Age, years | 69 [58–78] | 59 [46–72] | 71 [63–80] | .001 |
| Male sex, n (%) | 144 (53.9) | 38 (50.67) | 106 (55.21) | .503 |
| Weight, kg | 71 [62–83] | 72 [64–82] | 71 [62–83] | .919 |
| BMI, kg/m2 | 26.1 [23.2–29.4] | 25.8 [23.4–29.1] | 26.2 [23.2–29.4] | .938 |
| HTN | 149 (55.8) | 32 (42.3) | 117(60.9) | .007 |
| Lung disease | 49 (18.3) | 3 (4) | 46 (24.0) | .001 |
| Renal failure | 29 (11.0) | 2 (2.7) | 27 (14.1) | .007 |
| Renal impairment eGFR<30mL/min | 12 (4.5) | 1 (1.3) | 11 (5.7) | .119 |
| AD prediction | 44 (16.5) | 1 (1.3) | 43 (22.4) | .001 |
| Heart disease | 159 (59.6) | 44 (58.7) | 115 (59.9) | .854 |
| Valvulopathy | 100 (37.5) | 21 (28) | 79 (41.2) | .046 |
| EF<30% n (%) | 17 (6.4) | 1 (1.3) | 16 (8.3) | .036 |
| ASA | ||||
| I | 21 (7.9) | 15 (20) | 6 (3.1) | .001 |
| II | 89 (33.3) | 50 (66.7) | 39 (20.3) | |
| III | 129 (48.3) | 10 (13.3) | 119 (62.0) | |
| IV | 28 (10.5) | 0 (0) | 28 (14.6) | |
| TEE indication | ||||
| Structural planning | 87 (32.6) | 19 (25.3) | 68 (35.4) | .001 |
| Endocarditis | 76 (28.5) | 12 (16) | 64 (33.3) | |
| Stroke | 55 (20.6) | 33 (44) | 22 (11.5) | |
| Planning surgery | 17 (6.4) | 4 (5.3) | 13 (6.8) | |
| Structural control | 17 (6.4) | 4 (5.3) | 13 (6.8) | |
| EC | 3 (1.1) | 0 (0) | 3 (1.6) | |
| Prosthetic thrombosis | 6 (2.3) | 2 (2.7) | 4 (2.1) | |
| Other thrombosis | 5 (1.9) | 1 (1.3) | 4 (2.1) | |
| Mass studies | 1 (0.4) | 0 (0) | 1 (0.5) | |
AD, airway difficult; AP, anesthesiology professionals; ASA, American Society of Anesthesiologists Physical Status Classification System Scale; BMI, body mass index; EC, electrical cardioversion; EF, ejection fraction; eGFR, estimated glomerular filtration rate; HTN, hypertension; NAP, non-anesthesiologist professionals; TEE, transesophageal echocardiography.
Data are expressed as no. (%), mean±standard deviation or median [interquartile range]. P values<.05 are bolded.
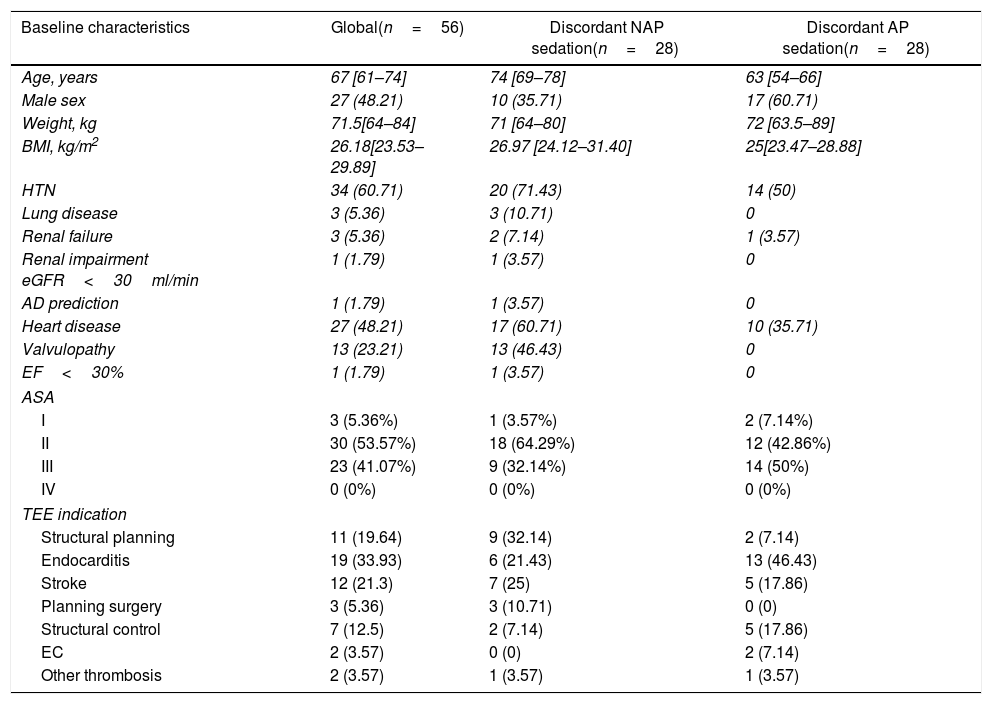
Out of the total study sample 28 patients with NAP sedation criteria were sedated by AP (discordant AP sedation) and conversely, 28 of the patients with AP sedation criteria were sedated by NAP (discordant NAP sedation), as detailed in Table 2.
Characteristics of discordant cases.
| Baseline characteristics | Global(n=56) | Discordant NAP sedation(n=28) | Discordant AP sedation(n=28) |
|---|---|---|---|
| Age, years | 67 [61–74] | 74 [69–78] | 63 [54–66] |
| Male sex | 27 (48.21) | 10 (35.71) | 17 (60.71) |
| Weight, kg | 71.5[64–84] | 71 [64–80] | 72 [63.5–89] |
| BMI, kg/m2 | 26.18[23.53–29.89] | 26.97 [24.12–31.40] | 25[23.47–28.88] |
| HTN | 34 (60.71) | 20 (71.43) | 14 (50) |
| Lung disease | 3 (5.36) | 3 (10.71) | 0 |
| Renal failure | 3 (5.36) | 2 (7.14) | 1 (3.57) |
| Renal impairment eGFR<30ml/min | 1 (1.79) | 1 (3.57) | 0 |
| AD prediction | 1 (1.79) | 1 (3.57) | 0 |
| Heart disease | 27 (48.21) | 17 (60.71) | 10 (35.71) |
| Valvulopathy | 13 (23.21) | 13 (46.43) | 0 |
| EF<30% | 1 (1.79) | 1 (3.57) | 0 |
| ASA | |||
| I | 3 (5.36%) | 1 (3.57%) | 2 (7.14%) |
| II | 30 (53.57%) | 18 (64.29%) | 12 (42.86%) |
| III | 23 (41.07%) | 9 (32.14%) | 14 (50%) |
| IV | 0 (0%) | 0 (0%) | 0 (0%) |
| TEE indication | |||
| Structural planning | 11 (19.64) | 9 (32.14) | 2 (7.14) |
| Endocarditis | 19 (33.93) | 6 (21.43) | 13 (46.43) |
| Stroke | 12 (21.3) | 7 (25) | 5 (17.86) |
| Planning surgery | 3 (5.36) | 3 (10.71) | 0 (0) |
| Structural control | 7 (12.5) | 2 (7.14) | 5 (17.86) |
| EC | 2 (3.57) | 0 (0) | 2 (7.14) |
| Other thrombosis | 2 (3.57) | 1 (3.57) | 1 (3.57) |
AD, airway difficult; AP, anesthesiology professionals; ASA, American Society of Anesthesiologists Physical Status Classification System Scale; BMI, body mass index; EC, electrical cardioversion; EF, ejection fraction; eGFR, estimated glomerular filtration rate; HTN, hypertension; NAP, non-anesthesiologist professionals; TEE, transesophageal echocardiography.
Data are expressed as no. (%), mean±standard deviation or median [interquartile range].
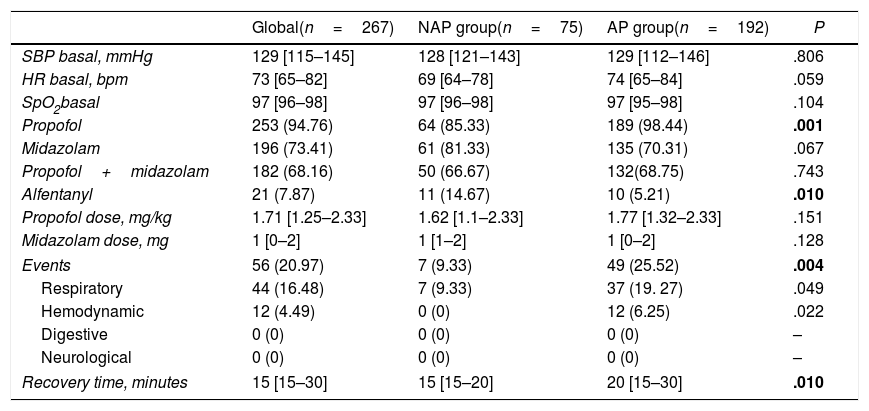
Procedure sedation results are summarized in Table 3. Baseline vital signs were similar in both groups. Propofol was the main drug used (85% NAP vs 98% AP) at a similar mean dose of 1.71mg/kg and combined with midazolam in 68% of cases. The event rate was higher in the AP sedated group. The overall event rate was 21% and respiratory and global hemodynamics events were 16.5% and 4.5%, respectively. EI or cardiopulmonary resuscitation maneuvers were not necessary in any case. The rate of digestive or neurological events in both groups was 0%.
Sedation procedure.
| Global(n=267) | NAP group(n=75) | AP group(n=192) | P | |
|---|---|---|---|---|
| SBP basal, mmHg | 129 [115–145] | 128 [121–143] | 129 [112–146] | .806 |
| HR basal, bpm | 73 [65–82] | 69 [64–78] | 74 [65–84] | .059 |
| SpO2basal | 97 [96–98] | 97 [96–98] | 97 [95–98] | .104 |
| Propofol | 253 (94.76) | 64 (85.33) | 189 (98.44) | .001 |
| Midazolam | 196 (73.41) | 61 (81.33) | 135 (70.31) | .067 |
| Propofol+midazolam | 182 (68.16) | 50 (66.67) | 132(68.75) | .743 |
| Alfentanyl | 21 (7.87) | 11 (14.67) | 10 (5.21) | .010 |
| Propofol dose, mg/kg | 1.71 [1.25–2.33] | 1.62 [1.1–2.33] | 1.77 [1.32–2.33] | .151 |
| Midazolam dose, mg | 1 [0–2] | 1 [1–2] | 1 [0–2] | .128 |
| Events | 56 (20.97) | 7 (9.33) | 49 (25.52) | .004 |
| Respiratory | 44 (16.48) | 7 (9.33) | 37 (19. 27) | .049 |
| Hemodynamic | 12 (4.49) | 0 (0) | 12 (6.25) | .022 |
| Digestive | 0 (0) | 0 (0) | 0 (0) | – |
| Neurological | 0 (0) | 0 (0) | 0 (0) | – |
| Recovery time, minutes | 15 [15–30] | 15 [15–20] | 20 [15–30] | .010 |
AP, anesthesiology professionals; HR, heart rate; SBP, systolic blood pressure; NAP, non-anesthesiology professionals.
Data are expressed as no. (%), mean±standard deviation or median [interquartile range]. P values<.05 are bolded.
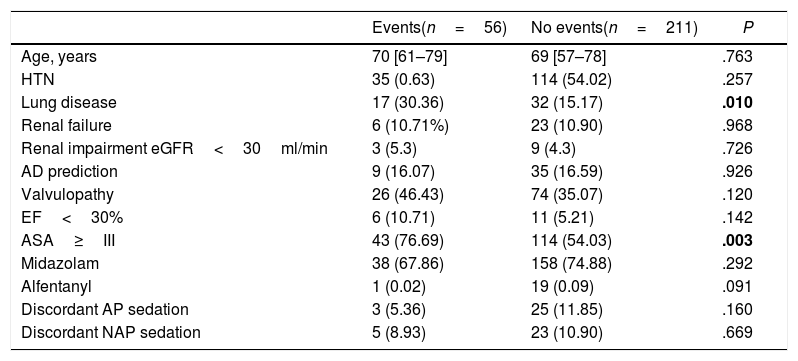
Global event rate was associated with the presence of previous lung disease and with ASA grade≥III. The other variables included in the algorithm as well as significant differences in baseline characteristics and discordant NAP group sedation were not associated with events (Table 4). In the multivariate analysis, sedation by NAP group had a tendency to reduce events (OR, 0.49; 95%CI, 0.18–1.3) regardless of ASA degree (Table 5).
Group features with events.
| Events(n=56) | No events(n=211) | P | |
|---|---|---|---|
| Age, years | 70 [61–79] | 69 [57–78] | .763 |
| HTN | 35 (0.63) | 114 (54.02) | .257 |
| Lung disease | 17 (30.36) | 32 (15.17) | .010 |
| Renal failure | 6 (10.71%) | 23 (10.90) | .968 |
| Renal impairment eGFR<30ml/min | 3 (5.3) | 9 (4.3) | .726 |
| AD prediction | 9 (16.07) | 35 (16.59) | .926 |
| Valvulopathy | 26 (46.43) | 74 (35.07) | .120 |
| EF<30% | 6 (10.71) | 11 (5.21) | .142 |
| ASA≥III | 43 (76.69) | 114 (54.03) | .003 |
| Midazolam | 38 (67.86) | 158 (74.88) | .292 |
| Alfentanyl | 1 (0.02) | 19 (0.09) | .091 |
| Discordant AP sedation | 3 (5.36) | 25 (11.85) | .160 |
| Discordant NAP sedation | 5 (8.93) | 23 (10.90) | .669 |
AD, airway difficult; AP, anesthesiology professionals; ASA, American Society of Anesthesiologists Physical Status Classification System Scale; EF, ejection fraction; eGFR, glomerular filtration rate; HTN, hypertension; NAP, non-anesthesiology professionals.
Data are expressed as no. (%), mean±standard deviation or median [interquartile range]. P values<.05 are bolded.
Urgent Anesthesiology support was required in only one case, due to difficulty in the introduction of the TEE probe. Recovery time after sedation was 20min in the AP group, and 15min in the NAP group.
DiscussionMost relevant findings of the studyUpdate in the transesophageal echocardiography indicationsThe results of our study confirm a change in the indication for TEE studies, with a high demand for those aimed at planning and evaluating percutaneous and surgical interventional procedures (45.3% of all studies). These studies are usually more extensive and detailed, as they require a methodical and careful assessment that should not depend on the patient's tolerance. Moreover, many of these patients would need follow-up studies; in this sense, a pleasant memory by means of sedation facilitates this continuity.
Safety of moderate sedation with propofol by NAPOur work shows the safety of a TEE program with moderate propofol sedation designed in collaboration with the Anesthesiology department and carried out by NAP, based on the appropriate selection of patients and identification of those with a higher risk of complications.
The safety of midazolam in TEE studies is well known from two randomized trials. The first, by the group by Aeschbacher et al.11 and including 200 patients, demonstrated the safety of midazolam with only 3% of desaturation episodes (SpO2<90%). The other was performed by Blondheim et al.12 on 62 patients, showing an incidence of respiratory events of 23%. None of the patients in these studies required EI and in both there were statistically significant differences in terms of tolerance to the procedure facilitated by sedation.
Safety with the use of propofol in TEE has been less well characterized. There are 2 studies with few patients. The first, from Ferson et al.,13 compared 8 patients with NAP-administered midazolam and 34 patients AP-administered propofol. It identified a rate of respiratory events (SpO2<90%) between the midazolam and the propofol group of 12.5% vs 17.6% and a striking rate of incomplete studies of 37.5% vs 0%. The second study, by Toman et al.,5 compared 3 therapies: midazolam (M), midazolam-alfentanil (MA), and propofol (P), administered by AP. They observed a respiratory event rate (SpO2<90%) of 13.3% vs 0.03% vs 16.7% in M, MA and P, respectively, without statistically significant differences.
In this line, our work provides information on the incidence of events with the use of midazolam+propofol for TEE procedures performed by NAP, which was found to be around 21% globally, 16.5% for respiratory events and 4.5% for hemodynamic events. All complications were mild and did not require invasive rescue procedures such as EI, nor hospitalization. Events were mainly related to the presence of previous lung disease and higher comorbidity, as reflected by an ASA degree≥III. Therefore, our findings underscore that patient selection is key to achieving a low complication rate when sedation is performed by non-anesthesiologists.
Protocol safety and efficacyThere was a crossover of 56 patients between the two initially defined groups, probably due to errors in the functioning of the circuit in its first year. Characteristics of the discordant patients are detailed in Table 2. Safety in the group of 56 discordant patients, and particularly in the subgroup of 28 patients assigned to AP sedation but sedated by NAP was tested. The global prevalence of complications in the 56-patients discordant group was 3%, whereas the prevalence of complications in the discordant subgroup sedated by NAP was 1.87%. We did not detect a significant increase in complications in misclassified patients.
Clinical implicationsThe results of this study show the expansion of TEE in cardiac imaging units, with a new profile of patients with advanced heart disease directed to percutaneous or surgical intervention. This may require the reorganization of the units to respond to new demands, including the establishment of collaboration circuits between medical specialties as well as the incorporation of cardiac imaging specialists trained in the interventionist field. Also, our safety data support the expansion of propofol sedation in TEE procedures performed by NAPs in selected patients.
LimitationsOur work is a registry of patients included in a pilot sedation program with a selection algorithm that results in two clearly differentiated groups. This may limit the comparability of results between the 2 groups. However, safety data, events and recovery time are similar to previously published work.
Moreover, a standardized definition and classification of adverse events has not been used, thus limiting the comparison with other studies.
ConclusionsModerate propofol sedation in transesophageal echocardiography procedures performed by trained non-anesthesiologist personnel is safe after adequate patient selection. The creation of these collaboration agreements between specialists could serve to extend sedation to all patients undergoing TEE in a safe and protocolized manner, increasing the efficiency of available resources and reducing waiting lists and healthcare pressure on Cardiology and Anesthesiology services.
- -
Main indications for TEE studies are stroke and endocarditis.
- -
Sedation for TEE studies with midazolam is safe but less deep..
- -
Sedation with propofol is deeper, with a higher complication rate.
- -
The safety level of sedation with propofol performed by cardiologists for TEE studies is unknown.
- -
Main indications for TEE in our center are planning and follow-up studies for percutaneous and surgical cardiac interventions.
- -
Sedation with propofol performed by cardiologists for TEE studies is safe in selected patients with advanced heart disease.
- -
Previous lung disease and ASA grade≥III were related to a higher risk of events.
None.
Authors’ contributionsC.H. Li: concept/design, data analysis/interpretation, drafting article, critical revision of article, approval of article, statistics, data collection; V. González-Salvado: data analysis/interpretation, drafting article; E. Bertolí: drafting article, data collection; D. Viladés: drafting article, data analysis/interpretation; M. Descalzo: data analysis/interpretation; F. Carreras: data analysis/interpretation; R. Leta: data analysis/interpretation; J. Cinca: critical revision of article; H. Capellades: data collection, concept/design; L. Cueva: concept/design; and P. Paniagua: drafting article, concept/design.
Conflicts of interestNone.
Abbreviations: TEE, transesophageal echocardiography; NAP, non-anesthesiologist professional; AP, anesthesiologists professional.