Out-of-hospital cardiac arrest (OHCA) is a leading cause of death worldwide. Survival after OHCA is poor, although it has improved in the last decade because of the availability of public access to defibrillators.1 European guidelines2 recommend an implantable cardioverter defibrillator (ICD) in patients with OHCA and a documented ventricular fibrillation in the absence of reversible causes such as acute coronary syndrome (ACS). However, there is limited data available on the use of an ICD in this group of patients.3,4
Also, in patients with OHCA and evidence of coronary artery disease (CAD), it can be difficult to determine whether or not ACS is the cause of the cardiac arrest. Thus, the indication of ICD implantation could be difficult to assess in certain specific post-OHCA scenarios.
Therefore, we analyzed a cohort of our tertiary-care hospital with ICD implantation after an OHCA, in order to assess the phenotype of such patients and the use, prognosis, and complications related to ICD implantation during follow-up. We also studied the presence of CAD in this population in order to know if there was any difference in outcomes.
We carried out a pilot observational retrospective study of a cohort of patients surviving an OHCA who were admitted to our center between January 2008 and December 2017, and that had an ICD implanted before hospital discharge. The study adhered to the principles of the Declaration of Helsinki. The ethics comitee or our centre aproved the study and informed consent was waived. Exclusion criteria were the presence of a previously implanted ICD, ACS in the previous 48h (except when ICD was indicated due to left ventricular dysfunction), poor neurological prognosis (cerebral performance category 3–5), or in-hospital death before ICD implantation. We reviewed clinical reports about baseline characteristics, left ventricle ejection fraction (LVEF) assessed by echocardiography, hospitalization data and follow-up. As noted, we divided the total cohort of patients in 2 different groups, with and without obstructive CAD (defined as previous revascularization or presence of coronary artery stenosis of > 50% in the left main or > 70% in other arteries), and we assessed the outcomes in terms of mortality, ventricular arrhythmia and ICD therapies.
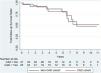
Categorical variables are presented as percentages, assessing the differences by the chi-square test (or Fisher test when necessary). Continuous variables are presented as a mean±standard deviation (SD) or as a median [interquartile range]. Survival Kaplan–Meier curves were constructed. Cox proportional hazard regression was used to calculate the non-standardized incidence rate per 100 person-years of outcomes at maximum follow-up. Analyses were performed using STATA software (V 14.0, StataCorp-LP, United States).
The first part of Table 1 shows baseline clinical characteristics of the population and data from the clinical presentation of the OHCA event. During the 10-year study period, a total of 1603 ICD were implanted. Of them, 62 (4%) were implanted after an OHCA hospitalized at our center (70% male, mean age 61.4±2.2 years). The median follow-up length was 5 years (59 months) [range 12–108]. Twelve patients (19%) had an ICD indication as primary prevention prior to index OHCA. Most of the patients (60%) did not have CAD. Emergent catheterization was performed in 35 patients (56%), of which 7 (11% of the total cohort) had ST segment elevation on the electrocardiogram (ECG), but only one of them showed an acute thrombotic occlusion (ATO) in the coronary angiography. However, 4 patients (6.4%) presented with ATO without ST segment elevation on electrocardiograms. Time to return of spontaneous circulation was longer in the CAD group than in the non-CAD group. Patients with CAD showed a trend to a lower LVEF at discharge.
Clinical characteristics and main outcomes.
| Overall | CAD cohort | Non-CAD cohort | P | |
|---|---|---|---|---|
| (n=62) | (n=25) | (n=37) | ||
| Baseline characteristics | ||||
| Age (years) | 61.4±2.2 | 64.5±3.4 | 59.3±2.1 | .25 |
| Male | 48 (77) | 22 (88) | 26 (70) | .10 |
| Hypertension | 38 (61) | 17 (68) | 21 (56) | .43 |
| Hyperlipidemia | 27 (43) | 13 (52) | 14 (37) | .30 |
| Diabetes mellitus | 36 (58) | 14 (56) | 22 (59) | .79 |
| Smoker or previous smoker | 30 (48) | 15 (60) | 15 (40) | .19 |
| Family history of sudden death | 6 (10) | 1 (4) | 5 (14) | .38 |
| Family history of MI | 6 (10) | 3 (12) | 3 (8) | .67 |
| Previous cardiovascular disease | ||||
| Prior MI | 17 (27) | 17 (74) | 0 (0) | NA |
| Previous PCI | 13 (21) | 13 (54) | 0 (0) | NA |
| Previous CABG | 6 (10) | 6 (26) | 0 (0) | NA |
| NYHA class | .04 | |||
| I | 15 (43) | 3 (20) | 12 (60) | |
| II | 15 (43) | 8 (53) | 7 (35) | |
| III | 5 (14) | 4 (26) | 1 (5) | |
| IV | 0 (0) | 0 (0) | 0 (0) | |
| Previous LVEF (%) | .11 | |||
| > 55 | 9 (15) | 3 (12) | 6 (16) | |
| > 35 | 16 (26) | 7 (28) | 9 (24) | |
| < 35 | 12 (19) | 7 (28) | 5 (13) | |
| Unknown | 25 (40) | 8 (32) | 17 (45) | |
| Hospitalization data | ||||
| ROSC (min) | 13.2±1.3 | 7.8±1.3 | 17±1.9 | .001 |
| ST-elevation segment on first | 7 (11) | 2 (8) | 5 (14) | .51 |
| ECG | ||||
| Emergent catheterization | 35 (56) | 15 (60) | 20 (54) | .001 |
| Acute thrombotic occlusion | 5 (20) | 0 (0) | NA | |
| LVEF at discharge (%) | 40.3±1.9 | 35.9±12.6 | 43.2±16.2 | .06 |
| LGE CMR | 19 (46) | 12 (67) | 7 (30) | .02 |
| NYHA≥3 at discharge | 6 (16) | 2 (18) | 4 (14) | .81 |
| Medical treatment at discharge | ||||
| Beta-blockers | 49 (80) | 19 (79) | 30 (81) | .81 |
| Amiodarone | 15 (24) | 8 (24) | 7 (19) | .22 |
| ICD-implant-related complications | 6 (10) | 3 (12) | 3 (9) | .6 |
| Outcomes | ||||
| 1 year all-cause mortality | 4 (7) | 1 (4) | 3 (9) | .63 |
| Median follow-up | 5.1 (2.4–8) | 4.6 (2.6–8.6) | 5.1 (2.4–7.9) | .44 |
| All-cause mortality (%/year) | 5.2 | 5.3 | 5.2 | .48 |
| Ventricular arrhythmia (%/year) | 5.9 | 6.7 | 5.2 | .31 |
| Appropriate shock (%/year) | 3.4 | 3.1 | 3.7 | .40 |
| Appropriate ATP (%/year) | 4.6 | 5.5 | 3.9 | .27 |
| Inappropriate shock (%/year) | 0.3 | 0 | 0.6 | .28 |
| Inappropriate ATP (%/year) | 0.3 | 0 | 0.6 | .28 |
| ICD-related complications (%/year) | 0.6 | 0.8 | 0.6 | .43 |
Values are n (%) or mean± standard deviation. ATP, antitachycardia pacing; CAD, coronary artery disease; CABG, coronary artery bypass grafting; CMR, cardiovascular magnetic resonance; ICD, implantable cardioverter-defibrillator; LGE, late gadolinium enhancement; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NA, not applicable; PCI, percutaneous coronary intervention; ROSC, return of spontaneous circulation.
Main outcomes in the overall population and the predefined subgroups are described on the bottom part of Table 1. After ICD placement, only 1 patient (1.6%) died before hospital discharge (due to sepsis unrelated to the device). All-cause mortality rate was 5.2%/year in overall population with non-significant differences between both subgroups (5.3%/year and 5.2%/year in CAD and non-CAD groups, respectively), mainly due to non-cardiovascular causes. Fig. 1 shows survival Kaplan–Meier curves in CAD and non-CAD groups. More than a quarter of the patients (27%) had at least 1 episode of ventricular arrhythmia, requiring either appropriate ICD shock or anti-tachycardia pacing, again without significant differences when comparing both groups (3.1%/year and 3.7%/year, respectively, for shock therapy and 5.5%/year and 3.9%/year, respectively, for anti-tachycardia therapy). In 6 patients (37.5% of deaths) an appropriate therapy (shock or antitachycardia pacing [ATP]) preceded death with a mean time of 16.6±6.1 months (min 8.3, max 23.1). Only 2 patients (1 in each group) presented with ICD-related complications (lead dysfunction), none of them fatal.
There are 3 main observations summarized as follows. First, a high percentage of patients (19%) met the criteria for ICD placement as primary prevention before presenting with OHCA. Had this indication been implemented, the OHCA would likely have been avoided; specifically, functional class II–IV and LVEF less than 35% despite optimal medical treatment. A recent meta-analysis5 found that ICD placement reduced mortality by 24% (hazard ratio,0.76; 95% confidence interval (95%CI), 0.60–0.96; P=.02) in patients with CAD and left ventricular systolic dysfunction. Contradictory results in different studies have limited the conclusions with respect to patients without CAD and left ventricular systolic dysfunction. Second, our study underlines the difficulties in determining whether an ACS is the main cause of OHCA. Emergent catheterization was performed in more than half of our patients but only 11% of them met strict ST-elevation myocardial infarction (STEMI) criteria and only 1 of them had an ATO in the coronary angiography. However, 6.4% of patients presented an ATO without STEMI criteria. Nowadays, performing an emergent coronary angiogram after OHCA in patients without STEMI criteria is a controversial issue. Ongoing studies, such as the COUPE trial,6 are currently exploring this important question. And third, more than a quarter of our cohort presented with new ventricular arrhythmias after hospital discharge. Thus, the ICD was beneficial because these events were aborted by appropriate shock or ATP therapies, and patients who were treated by ICD and died did so a long time after ICD therapy. This benefit was observed regardless of the presence or absence of CAD. Both 1-year mortality and ICD-related complications during follow-up were low, which increased the net ICD benefit in this cohort of patients. The placement of an ICD as secondary prevention after OHCA with survival to discharge is underutilized; Ho et al. described an overall rate of 23.9%. Of 256 patients classified as “likely ICD-eligible”, 57.0% received an ICD. Admission to a hospital with ICD facilities was associated with a higher probability of implantation (odds ratio,2.85; 95%CI, 1.40–5.82).4 On the other hand, earlier implantation than the recommended by the guidelines (≤ 40 days post-myocardial infarction out-of-hospital cardiac arrest) has been associated with a long-term survival benefit.3 This may be especially beneficial in patients with CAD, in whom we cannot determine whether or not ACS was the cause of the OHCA.
The main limitation of this one-center study is the reduced sample size and its retrospective observational design, which comes with an inherent selection bias, and makes the study hypothesis-generating. Despite this, the results add clinical value as they reflect real-life practice and confirm under-prescription of ICD, both in primary and secondary prevention. Scarce data have been published about long-term follow-up outcomes of patients surviving an OHCA, with a subsequent prolonged hospitalization, and with a final ICD implantation.
In conclusion, in a long-term follow-up, survivors of an OHCA who received an ICD before hospital discharge showed a high number of arrhythmic events and appropriate post-implantation therapies, regardless of presenting CAD or not. The number of inappropriate shocks and ICD-related complications was low. The use of an ICD as primary prevention, according to current guidelines, could likely have prevented OHCA in a notable percentage of patients in our cohort.
FundingThis study has not received specific aid from agencies from de public sector, commercial sector, and non-profit entities.
Conflicts of interestNone.