Patients with angina pectoris despite angiographically unobstructed coronary arteries represent a diagnostic and therapeutic challenge. Coronary artery spasm (CAS) is an established cause of chest pain in patients with stable angina and unobstructed coronary arteries. Recent data have shown that approximately 50% of patients undergoing diagnostic coronary angiography for the assessment of typical chest pain have unobstructed coronary arteries and that CAS can be found in approximately 60% of such patients.1 These functional coronary vasomotor disorders may occur at the focal or diffuse epicardial level or in the microvasculature. However, the underlying pathomechanisms are still partially understood and data on circulating immune cells contributing to CAS is scarce. It has been shown that an unusual subset of T lymphocytes, characterized by the lack of CD28 receptor expression (CD4+CD28NULL T cells) are expanded in patients with acute coronary syndrome.2 It is believed that this T-cell subset can exert high proinflammatory (e.g. by high production of interferon-γ) and cytolytic properties leading to endothelial dysfunction and promotion of vascular inflammation. To the best of our knowledge, the role of CD4+CD28NULL T cells has not been investigated in patients with vasospastic angina. Thus, the aim of this study is to assess whether expansion of CD4+CD28NULL T cells is associated with CAS.
To address this issue 27 consecutive patients (19 men, age 57±15 years) with stable angina despite angiographically unobstructed coronary arteries (< 50% stenosis) who underwent intracoronary acetylcholine (ACh) testing for the diagnosis of CAS were assessed between November 2014 and June 2015 within a substudy of the ACOVA trial.1 All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants included in the study. For inclusion in the study, patients had to have symptoms suggestive of coronary artery disease (chest pain or dyspnoea, with or without occasional attacks of resting chest pain) with a positive result in the ACh-test. Patients with chronic obstructive pulmonary disease, cardiomyopathy, severe valvular heart disease, myocardial infarction within the last 3 months, or chronic inflammatory conditions (e.g. rheumatoid arthritis, lupus, etc.) were not included in the study. The ACh-test was performed directly after diagnostic coronary angiography according to a standardized protocol.3 Patients were classified according to the presence of focal (diameter reduction ≥ 90% in only one segment) or diffuse (diameter reduction ≥ 90% in ≥ 2 adjacent coronary segments) “epicardial coronary artery spasm” or “microvascular spasm” (no relevant changes of epicardial vessel diameter < 90%; see also Fig. 1). Because other studies have described a worse clinical outcome associated with focal coronary artery spasm in vasospastic angina,4 the patients in the present study were divided into two groups. Group 1 comprised patients with focal epicardial coronary spasm (focal spasm) and group 2 comprised patients with diffuse or microvascular spasm (non-focal spasm). In addition, the following information was recorded in every patient: gender, age at the date of the assessment, clinical presentation and traditional cardiovascular risk factors.
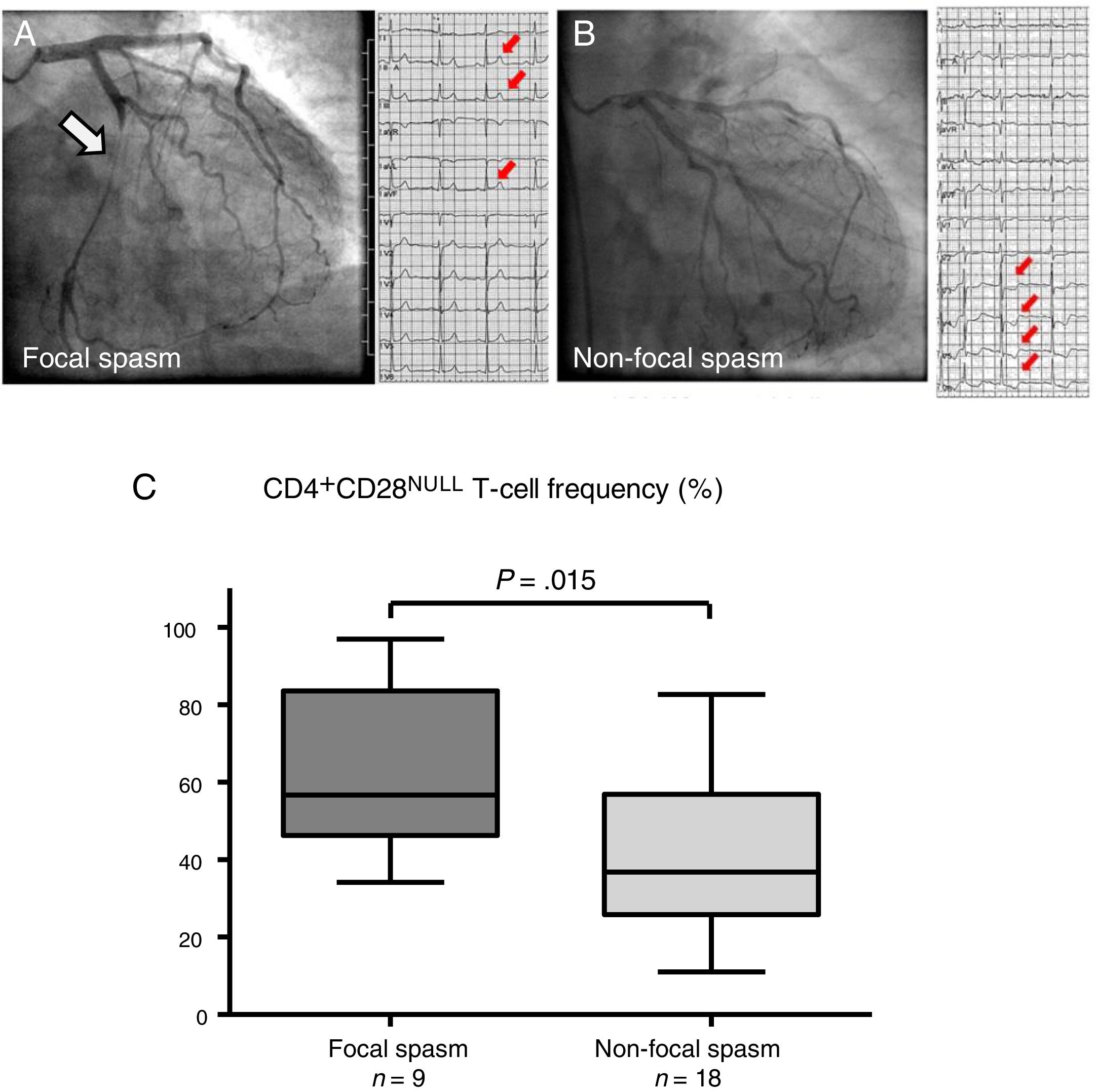
(A) Left coronary artery angiograms and electrocardiograms (ECGs) of a representative patient with epicardial focal spasm: In the left circumflex artery epicardial focal spasm (white arrow) was provoked by 100μg intracoronary (i.c.) acetylcholine (ACh) with concomitant ST-segment elevation (small arrows) and reproduction of the usual symptoms. (B) Left coronary artery angiograms and ECGs in a representative patient with non-focal (microvascular) spasm: During 100μg i.c. ACh infusion the patient showed reproduction of the usual symptoms with concomitant ST-segment depression (small arrows), but no relevant epicardial vasoconstriction. (C) Statistical analysis revealed that patients with focal coronary spasm had a significantly higher frequency of CD4+CD28NULL T cells compared to patients without focal spasm. Data are presented as box plots displaying medians, 25th and 75th percentiles (boxes) with Min/Max whiskers. Angiograms and ECGs in this figure have been previously published in Ong et al.3
Expansion of CD4+CD28NULL T cells in peripheral venous blood (EDTA whole blood samples) was directly analyzed and evaluated on the same day of blood collection on the flow cytometer BD FACSVerse using BD FACSuite Software (BD Biosciences, Germany). Non-specific, false-positive antibody staining was blocked using FcR-blocking reagent (Human BD Fc Block, BD Biosciences) for 10min at room temperature. For each patient a volume of 50μL blood sample per tube was incubated with antibodies against CD4 (PerCP mouse anti-human CD4 Clone SK3, #345770; BD Biosciences) and CD28 (BV421 mouse anti-human CD28 Clone CD28.2, #562613; BD Biosciences) for 20min, followed by a lysing step (Lysing buffer, BD Pharmingen; #555899) for 15min (both steps were carried out at room temperature protected from light according to the LNW method; lyse no wash method). For quantification of the measured events BD Trucount tubes were used (BD BioSciences; #340334) and verified with the implemented Flow Sensor. Autofluorescence- and isotype-controls were used to discriminate specific and non-specific antibody binding. Gates with the cells of interest were defined with the help of the single staining and the FMO control (Fluorescence Minus One) by exchanging the CD28-BV421 antibody with the corresponding isotype control IgG1-BV421. Acquisition was performed until a total number of 5000 BD Trucount bead were analyzed and the frequency of CD4+CD28NULL T cells was expressed as percentage of total CD4+ T cells.
Results are expressed as mean±standard deviation (SD). For statistical analysis of CD4+CD28NULL T cells the Student t test was used to compare normally distributed continuous variables, while Fisher's exact test was used for categorical variables. A two-tailed P<.05 was considered significant. Statistical data analysis was performed using SPSS 23.0 (IBM, USA).
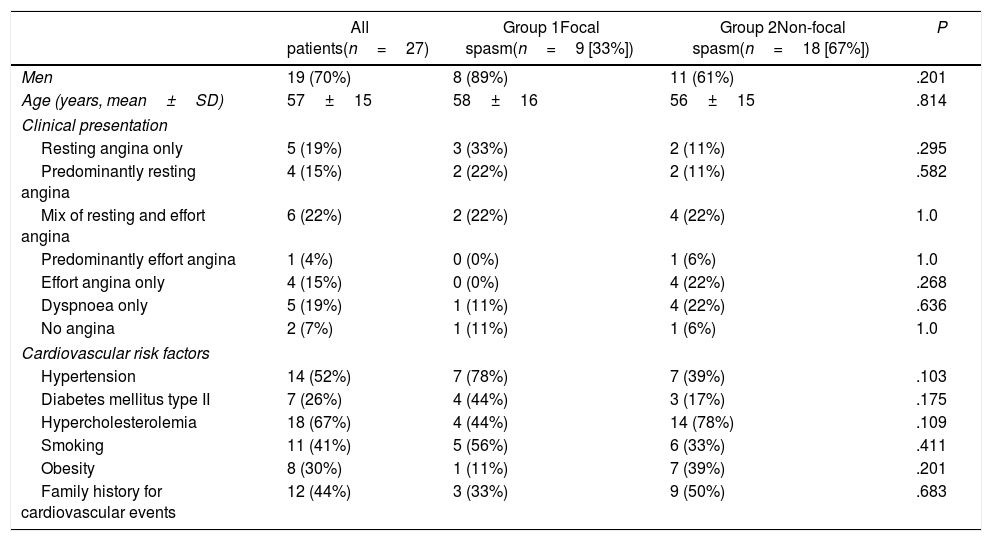
The ACh-test revealed epicardial spasm in 13 patients, 9 of them had focal and 4 had diffuse spasm. The remaining 14 patients had coronary microvascular spasm on ACh-testing. The clinical characteristics of the study patients are summarized in Table 1. Although 19 of 27 patients in our study cohort were men (70%), the proportion of male patients in group 1 (focal spasm) and group 2 (non-focal spasm) was not significantly different, 89% and 61%, respectively (P=.201). The comparison of age, clinical presentation (type of anginal symptoms) and cardiovascular risk factors revealed no statistically significant differences between patients with focal coronary spasm compared to patients with diffuse or microvascular spasm. As shown in Fig. 1, the frequency of CD4+CD28NULL T cells assessed via flow cytometry was significantly higher in patients with focal coronary spasm in comparison to the rest of the cohort (P=.015).
Clinical characteristics of the study patients.
| All patients(n=27) | Group 1Focal spasm(n=9 [33%]) | Group 2Non-focal spasm(n=18 [67%]) | P | |
|---|---|---|---|---|
| Men | 19 (70%) | 8 (89%) | 11 (61%) | .201 |
| Age (years, mean±SD) | 57±15 | 58±16 | 56±15 | .814 |
| Clinical presentation | ||||
| Resting angina only | 5 (19%) | 3 (33%) | 2 (11%) | .295 |
| Predominantly resting angina | 4 (15%) | 2 (22%) | 2 (11%) | .582 |
| Mix of resting and effort angina | 6 (22%) | 2 (22%) | 4 (22%) | 1.0 |
| Predominantly effort angina | 1 (4%) | 0 (0%) | 1 (6%) | 1.0 |
| Effort angina only | 4 (15%) | 0 (0%) | 4 (22%) | .268 |
| Dyspnoea only | 5 (19%) | 1 (11%) | 4 (22%) | .636 |
| No angina | 2 (7%) | 1 (11%) | 1 (6%) | 1.0 |
| Cardiovascular risk factors | ||||
| Hypertension | 14 (52%) | 7 (78%) | 7 (39%) | .103 |
| Diabetes mellitus type II | 7 (26%) | 4 (44%) | 3 (17%) | .175 |
| Hypercholesterolemia | 18 (67%) | 4 (44%) | 14 (78%) | .109 |
| Smoking | 11 (41%) | 5 (56%) | 6 (33%) | .411 |
| Obesity | 8 (30%) | 1 (11%) | 7 (39%) | .201 |
| Family history for cardiovascular events | 12 (44%) | 3 (33%) | 9 (50%) | .683 |
Data are expressed as no. (%) or mean±standard deviation.
In the present study we have shown for the first time that patients with focal epicardial spasm have a significantly greater expansion of CD4+CD28NULL T cells, an unusual subset of CD4+ T cells known to have high proinflammatory and cytotoxic properties, compared to patients without focal spasm. These findings may explain, at least in part, why other studies have described a worse clinical outcome associated with focal coronary spasm.4 This is further supported by other studies showing that CD4+CD28NULL T cell frequency is an independent predictor of future acute coronary events in patients with unstable angina.5 A caveat may lie in the fact that CD4+CD28NULL T cell expansion is related to age, a known marker for T cell senescence.6 However, the mean age in our cohort did not differ significantly between focal spasm compared to the rest of the cohort (58±16 years vs 56±15 years; P=.814). Therefore we can exclude that differences in age between the 2 groups might have influenced CD4+CD28NULL T cell frequency in our study. Furthermore, to rule out a possible contribution of chronic inflammatory disorders to CD4+CD28NULL T cell expansion, patients with chronic inflammatory conditions (e.g. rheumatoid arthritis) were excluded from the present study. The frequency of patients with diabetes was comparable between the 2 groups suggesting that this did not influence the differences in CD4+CD28NULL T cell frequency significantly (Table 1). A limitation of this study is the small patient cohort (n=27). A lager study population is necessary to confirm the results and to assess the clinical relevance by examination of CD4+CD28NULL T cell frequency in correlation with clinical outcome in patients with focal coronary spasm. Mechanistic in vitro studies suggest that the cytotoxic and inflammatory properties of CD4+CD28NULL T cells depend on their receptor profile, for example receptors of the killer immunoglobulin-like receptor family.2 Therefore further studies should characterize the functional properties and receptor profile of CD4+CD28NULL T cells expanded in patients with focal coronary spasm in more detail.
In conclusion, in the present study patients with focal epicardial spasm show a significantly greater expansion of CD4+CD28NULL T cells compared to patients with other coronary vasomotor disorders. This underlines the role of an inflammatory pathomechanism especially in patients with focal epicardial spasm. Further larger clinical trials are necessary to clarify whether modulation of CD4+CD28NULL T cells may represent a potential therapeutic target in the pathogenesis of CAS.
FundingThis study was partially supported by funds from the Robert-Bosch-Foundation and the Berthold-Leibinger-Foundation, Ditzingen, Germany. The authors have no financial interest in this article.
Conflicts of interestThe authors declare that they have no conflict of interest.
The authors are grateful to Sabine Nägele, study nurse, for her excellent support during the study.