Smoking has been related with lower short-term mortality among patients with acute myocardial infarction. This may be caused by different baseline characteristics, since smokers are significantly younger at the time of infarction. Our purpose was to study the smoking paradox focusing on age.
MethodsWe retrospectively studied 118 consecutive people aged<45 years and compared them to 236 patients aged 45–75 years, matched by sex and date of admission; all were admitted with an ST-segment elevation acute myocardial infarction (STEMI). Baseline characteristics, treatment patterns, cardiac catheterization parameters, in-hospital and 30 day-outcomes were thoroughly assessed and adjusted to the habit of smoking.
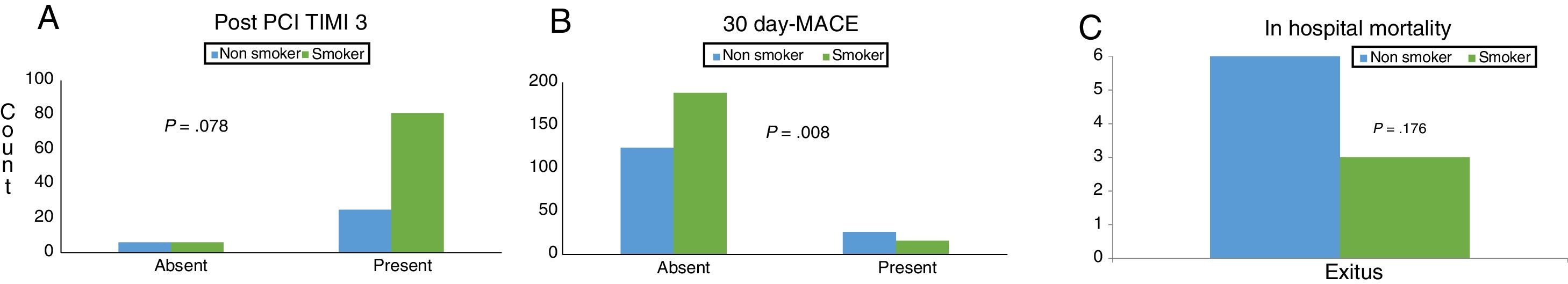
ResultsArterial hypertension and diabetes mellitus, were more frequent in the older group (P<.005). Advanced Killip grade on admission (P=.030) and decreased creatinine clearance (P < 0.001) were more frequent in the ≥ 45-year cohort. The younger cohort displayed a trend to have higher pre/post PCI TIMI 3 percentages, collaterals and a good myocardial perfusion after PCI. Stratifying by smoking habit, non-smokers presented more frequently hypertension (P=.037), diabetes (P=.039), higher Killip degrees and less TIMI 3 post-PCI (P=.078). Thus, the combined event (MACE) and reinfarctions tended to be more frequent in non-smokers (P=.052 and P=.055). The overall multivariate model revealed a 30-day MACE-relationship with smoking habit (OR, 0.918; 95%CI, 0.854–0.987, P=.020).
ConclusionsYoung smokers maintained the lower short-term events paradox. Our findings can contribute to explain the apparently different course of myocardial infarction in young people and point out a different mechanism of infarction in smokers.
Fumar se ha relacionado con menor mortalidad a corto plazo tras un infarto agudo de miocardio. Nuestro propósito fue estudiar esta paradoja tabáquica en función de la edad.
MétodosSe estudió retrospectivamente a 118 personas consecutivas de <45 años y las comparamos con 236 pacientes de 45-75 años, agrupados por sexo y fecha de ingreso; todos ingresaron con un infarto agudo de miocardio con elevación del segmento ST. Se analizaron las características basales, del tratamiento, los parámetros del cateterismo cardíaco y la evolución hospitalaria y a 30 días, ajustándose al hábito de fumar.
ResultadosLa hipertensión arterial y la diabetes mellitus fueron más frecuentes en el grupo de mayor edad (p <0,005). El grado avanzado de Killip al ingreso (p=0,030) y la disminución del aclaramiento de creatinina (p <0,001) fueron más frecuentes en ≥ 45 años. La cohorte más joven mostró una tendencia a tener>TIMI 3 de intervención coronaria pre/pospercutánea (ICP), colaterales y una buena perfusión miocárdica después del intervencionismo. Estratificando, los no fumadores presentaron con mayor frecuencia hipertensión (p=0,037), diabetes (p=0,039) más Killip y menos TIMI 3 después de PCI (p=0,078). Por lo tanto, el episodio combinado (acontecimientos cardiovasculares mayores) y reinfartos tendieron a ser más frecuentes en no fumadores (p=0,052 y p=0,055). El modelo multivariado reveló una relación de episodios cardiovasculares mayores a 30 días con el tabaco (OR=0,918; IC95%, 0,854-0,987; p=0,020).
ConclusionesLa paradoja tabáquica se observa también en menores de45 años, lo que apunta a un mecanismo diferente de infarto en los fumadores.
Although smoking is widely recognized as a major modifiable cardiovascular risk factor, its short-term influence on prognosis after myocardial infarction is by far less clear, showing a relationship previously widely known as the smoker's paradox.
Actually, smoking has been reported to be related with lower short term mortality among patients with acute myocardial infarction,1,2 stroke,3 and heart failure.4 This paradox may be caused by different baseline characteristics of smokers and nonsmokers,5 as significantly more young patients than older patients were smoker at the time of infarction.2,6 Thus, a number of studies were initially developed evaluating the effect of smoking on outcomes following revascularization for acute myocardial infarction,1,2,7–12 data on the differential effect of age remains lacking.
Our aim was to investigate the relationship between age and the effects of smoking in patients receiving an updated interventional approach after an ST-segment elevation acute myocardial infarction.
MethodsWe designed a paired-cohort single-center retrospective study which divided patients in two groups on the basis of age. Between March 2003 and February 2007 we included the complete cohort of 118 consecutive people aged < 45 years and compared them to 236 patients aged 45–75 years, matched by sex and date of admission, so every young patient had 2 older sex-matched pairs each. All of them had an ST-segment elevation acute myocardial infarction,13 and were admitted urgently to our coronary care unit for primary or rescue cardiac catheterization. Baseline characteristics, treatment patterns, in-hospital and 30 day-outcomes were collected and assessed adjusted to the habit of smoking (current active smoking). Localization of infarction was considered as anterior or non-anterior. Hemodynamic status was graded according to the Killip's classification. Coronary flow was graded according to the Thrombolysis in Miocardial Infarction (TIMI) scale before and after percutaneous coronary intervention (PCI), and collateral circulation regarding the Rentrop classification. For the purpose of our study, a Rentrop grade 2–3 was considered acceptable.14 Among patients with successful primary angioplasty, 161 had angiograms of enough quality to analyze myocardial perfusion according to the TIMI perfusion scale (TMPG).15 Myocardial perfusion was graded as good (TMP 2–3) or poor (TMP 0–1).
During hospitalization and 30 day-follow-up, cardiovascular death and new myocardial infarction13 were considered the main end-points. A combined end point (major adverse cardiovascular event [MACE]) included death, reinfarction, heart failure, angina, stroke, cardiac rupture and shock. Cardiogenic shock or Killip IV was defined by the clinical criteria of the SHOCK trial16: systolic pressure less than 90mmHg or necessity of intravenous inotropes for more than 30min, together with hypoperfusion signs, including cold skin and diuresis under 30mL/h.
A long-term exploratory analysis was performed later on. Long-term follow-up was performed through office visits or directly contacting the patient or family by telephone. The last follow-up was conducted on September 2019.
Statistical methodsSPSS for Windows (SPSS, United States) was used for statistical intra group analysis and STATA (Statacorp, United States) was used to perform the nested analyses required between paired cohorts. Unless otherwise indicated, data are expressed as mean value±standard deviation. When necessary, due to dispersion of data, they are shown as median and interquartile range. Comparisons between groups were made with Pearson's Chi-square test for categorical variables and the Student t test or Mann–Whitney U test for continuous variables. To address overfitting the number of variables to be included, the multivariable analysis was reduced by using a pre-specified model including those variables significant or near significant after univariate analysis and other well known to be related with the outcome. Thus, group/age, smoke, hypertension, diabetes mellitus, renal dysfunction (creatinine clearance <60mL/h, calculated by Cockroft and Gault formula), previous myocardial revascularization, were the variables included in the final binary logistic regression models. Comparisons were considered significant in presence of a 2-sided P value<.05.
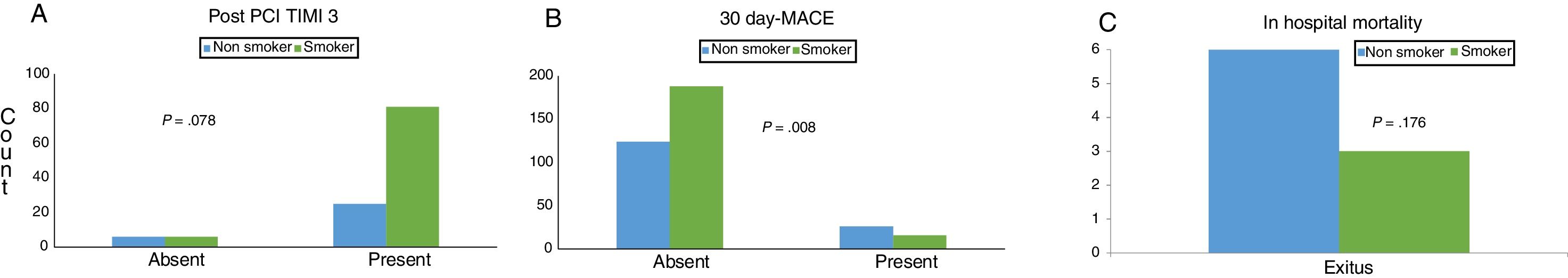
ResultsAn overall sample of 354 patients was finally enrolled in the study. Patient clinical characteristics at admission and clinical outcomes are shown in Table 1. Statistically significant differences between age groups were found in the percentage of smokers (73.7% vs 49.6%, P<.001), arterial hypertension (P=.005) and diabetes mellitus (P<.001); all more frequent in the older group. Advanced Killip grade on admission (P=.030) and decreased creatinine clearance (P<0.001) were more frequent in the ≥45 year-cohort, which presented a bigger infarction size assessed by peak CK (P=.017). Left ventricular ejection fraction was numerically superior in the younger group (P=.079). Anterior type infarction or multivesssel involvement did not reveal significant differences between groups. All patients underwent a cardiac catheterization procedure, 44 of them rescue PCI after failed thrombolysis.
Baseline, clinical, angiographic features and outcomes.
| Overall | <45 y | ≥45 y | P | |
|---|---|---|---|---|
| N | 354 | 118 | 236 | – |
| Smoker | 204 (57.6%) | 87 (73.7%) | 117 (49.6%) | <.001 |
| Age | 53.6±12.1 | 40.22±4.13 | 60.30±8.84 | – |
| Female | 45 (12.7%) | 15 (12.7%) | 30 (12.7%) | – |
| Hypertensiona | 142 (40.1%) | 32 (27.1%) | 110 (46.6%) | .005 |
| DMa | 67 (18.9%) | 13 (11.0%) | 54 (22.9%) | <.001 |
| Dyslipidemaa | 161 (45.5%) | 54 (45.8%) | 107 (45.3%) | 1.000 |
| Obesity | 75 (21.2%) | 26 (22.0%) | 49 (20.8%) | .410 |
| CR | 1.04±0.39 | 0.98±0.24 | 1.06±0.45 | .027 |
| CR clearance <60b | 37 (10.5%) | 2 (1.7%) | 35 (14.8%) | <.001 |
| Pre MI | 42 (11.9%) | 9 (7.6%) | 33 (14.0%) | .193 |
| Pre revascularization | 36 (10.2%) | 5 (4.2%) | 31 (13.2%) | .009 |
| Killip admission | ≥ II | 9 (7.6%) | 38 (16.6%) | .030 |
| I | 307 (86.7%) | 109 (92.4%) | 198 (83.9%) | |
| II | 37 (10.5%) | 7 (5.9%) | 30 (12.7%) | |
| III | 4 (1.1) | 1 (1.7%) | 2 (0.8%) | |
| IV | 6 (1.7%) | 0 | 6 (2.5%) | |
| Peak troponineIc | 54.6 (19.74–104.75) | 54.94 (21.84–107.17) | 54.62 (19.21–103.7) | .482 |
| PeakCKc | 1669.50 (752.50–3001.00) | 1939.00 (863.50–3221.00) | 1515 (683.00–2588.00) | .017 |
| LVEFd | 51.55±10.14 | 52.83±9.21 | 50.90±10.55 | .079 |
| AnteriorWe | 160 (40.2%) | 52 (44.1%) | 108 (45.8%) | .230 |
| In stay | 7.14±5.33 | 7.3±6.6 | 7.05±4.5 | .696 |
| Multivessel | 124 (35.5%) | 32 (27.1%) | 92 (38.9%) | .212 |
| TIMI 3 pre | 15.7% | 20.2% | 13.4% | .138 |
| TIMI 3 post | 86.3% | 89.8% | 84.0% | .340 |
| BlushOKf | 66.5% | 75.0% | 61.2% | .104 |
| Collateralsf | 52.8% | 60.0% | 49.0% | .211 |
| No reflow | 8.5% | 5.0% | 10.4% | .195 |
| 30 dayMACEg | 11.9% | 7.6% | 14.0% | .055 |
| Re MI30 dayg | 4.0% | 3.4% | 14.2% | .695 |
| Exitusg | 2.8% | 0% | 4.7% | .034 |
CK, creatinine kinase; DM, diabetes mellitus; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events; MI, myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction.
A good myocardial blush was considered when a TMPG>1 was present.15 Collaterals were considered when Rentrop scale was≥2.
The younger cohort displayed a trend to have higher pre and post-PCI TIMI 3 percentages (P=.144 and P=.181, respectively), see Table 1 and Fig. 1A. Collaterals (≥Rentrop 2) and a good myocardial perfusion (TMPG>1) after PCI had a trend to be more evident in the young group. Twenty-five patients developed non-reflow phenomenon during PCI, 15 (60%) of them with posterior complete immediate resolution; 67 patients received glycoprotein IIb/IIIa inhibitors, 29 patients required vasoactive drugs, 21 fulfilled cardiogenic shock criteria16 and 14 had reinfarction (during revascularization procedures or follow-up), without differences between age groups. Other complications were angina after discharge (3), stroke (1), papillary muscle rupture with severe mitral regurgitation (2), and admission due to heart failure (1), see Fig. 1B. During the first month, 10 patients died (9 in hospital, one of them due to a cardiac rupture), all in the ≥ 45-year group, as shown in Fig. 1C (P=.034).
Bar charts, stratified by tobacco consumption. (A) Post percutaneous coronary intervention (PCI) Thrombolysis in Myocardial Infarction (TIMI) 3 flow, in the younger group. (B) 30-Day combined events major adverse cardiovascular events (MACE). (C) In-hospital deaths. Last 2 graphs refer to the overall population.
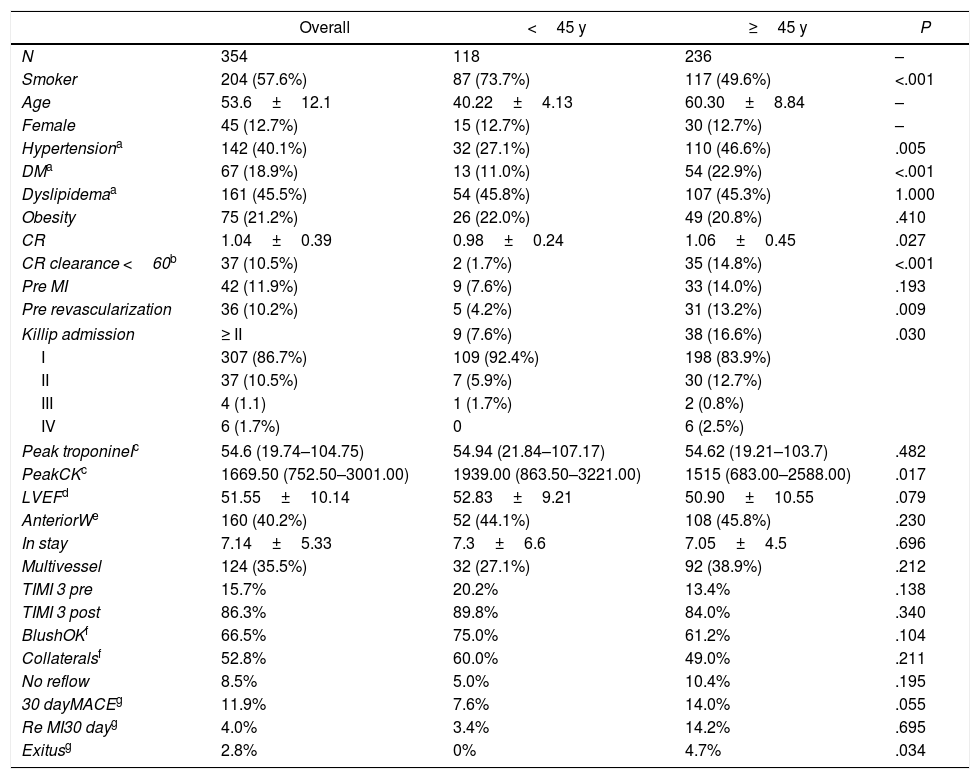
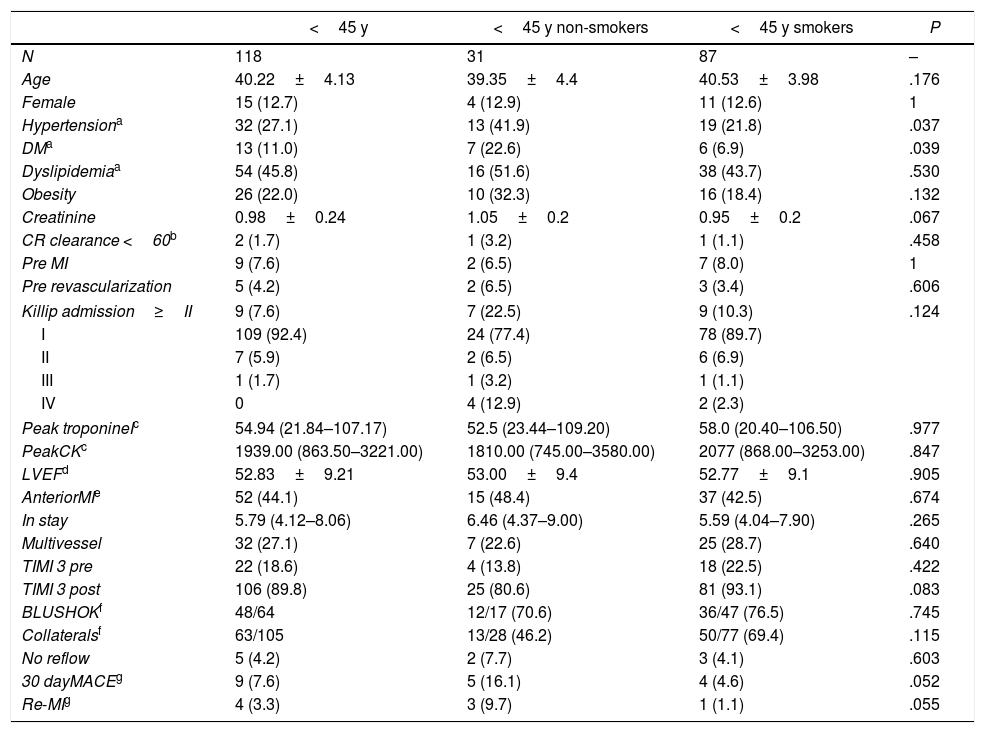
The analysis of the younger cohort is displayed in Table 2 and Fig. 2. After stratifying by smoking habit, non-smokers presented more frequently hypertension (P=.037), diabetes (P=.039), a trend for a higher Killip degree (P=.124) and less TIMI 3 post-PCI (80.6% vs 93.1%, P=.078). Other angiographic characteristics did not reach statistical significance (Fig. 2, and Table 2).
Baseline, clinical, angiographic features and outcomes in the young cohort.
| <45 y | <45 y non-smokers | <45 y smokers | P | |
|---|---|---|---|---|
| N | 118 | 31 | 87 | – |
| Age | 40.22±4.13 | 39.35±4.4 | 40.53±3.98 | .176 |
| Female | 15 (12.7) | 4 (12.9) | 11 (12.6) | 1 |
| Hypertensiona | 32 (27.1) | 13 (41.9) | 19 (21.8) | .037 |
| DMa | 13 (11.0) | 7 (22.6) | 6 (6.9) | .039 |
| Dyslipidemiaa | 54 (45.8) | 16 (51.6) | 38 (43.7) | .530 |
| Obesity | 26 (22.0) | 10 (32.3) | 16 (18.4) | .132 |
| Creatinine | 0.98±0.24 | 1.05±0.2 | 0.95±0.2 | .067 |
| CR clearance <60b | 2 (1.7) | 1 (3.2) | 1 (1.1) | .458 |
| Pre MI | 9 (7.6) | 2 (6.5) | 7 (8.0) | 1 |
| Pre revascularization | 5 (4.2) | 2 (6.5) | 3 (3.4) | .606 |
| Killip admission≥II | 9 (7.6) | 7 (22.5) | 9 (10.3) | .124 |
| I | 109 (92.4) | 24 (77.4) | 78 (89.7) | |
| II | 7 (5.9) | 2 (6.5) | 6 (6.9) | |
| III | 1 (1.7) | 1 (3.2) | 1 (1.1) | |
| IV | 0 | 4 (12.9) | 2 (2.3) | |
| Peak troponineIc | 54.94 (21.84–107.17) | 52.5 (23.44–109.20) | 58.0 (20.40–106.50) | .977 |
| PeakCKc | 1939.00 (863.50–3221.00) | 1810.00 (745.00–3580.00) | 2077 (868.00–3253.00) | .847 |
| LVEFd | 52.83±9.21 | 53.00±9.4 | 52.77±9.1 | .905 |
| AnteriorMIe | 52 (44.1) | 15 (48.4) | 37 (42.5) | .674 |
| In stay | 5.79 (4.12–8.06) | 6.46 (4.37–9.00) | 5.59 (4.04–7.90) | .265 |
| Multivessel | 32 (27.1) | 7 (22.6) | 25 (28.7) | .640 |
| TIMI 3 pre | 22 (18.6) | 4 (13.8) | 18 (22.5) | .422 |
| TIMI 3 post | 106 (89.8) | 25 (80.6) | 81 (93.1) | .083 |
| BLUSHOKf | 48/64 | 12/17 (70.6) | 36/47 (76.5) | .745 |
| Collateralsf | 63/105 | 13/28 (46.2) | 50/77 (69.4) | .115 |
| No reflow | 5 (4.2) | 2 (7.7) | 3 (4.1) | .603 |
| 30 dayMACEg | 9 (7.6) | 5 (16.1) | 4 (4.6) | .052 |
| Re-MIg | 4 (3.3) | 3 (9.7) | 1 (1.1) | .055 |
Patients are divided and compared by tobacco consumption.
Unless otherwise indicated, data are expressed as no. (%) or mean±standard deviation.
CK, creatinine kinase; DM, diabetes mellitus; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events;; MI, myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction.
A good myocardial blush was considered when a TMPG>1 was present15. Collaterals were considered when Rentrop scale was≥2.
Thus, the combined event (MACE) and the number of reinfarctions were numerically more frequent in non-smokers (16.1% vs 4.6%, P=.052 and 9.7% vs 1.1%, P=.055, respectively). There were no deaths in the younger cohort.
Fig. 2A shows better collaterals in young smokers compared to young non-smokers. Cardiovascular events were slightly superior in non-smokers (P=.008) but in-hospital mortality did not reach statistical signification (P=.176), Fig. 1B,C, respectively. Rescue PCI was numerically, but not statistically, more frequently needed in young non-smokers when compared with smokers matched by age (16.1% vs 13.8%, P=.7).
In the multivariate model, we included all variables previously exposed significant by the univariate analysis (creatinine clearance, previous revascularization, hypertension, diabetes, age group and smoking habit). The overall model revealed a slight relationship between MACE and smoking habit (odds ratio [OR], 0.918; 95% confidence interval [95%CI], 0.854–0.987, P=.020).
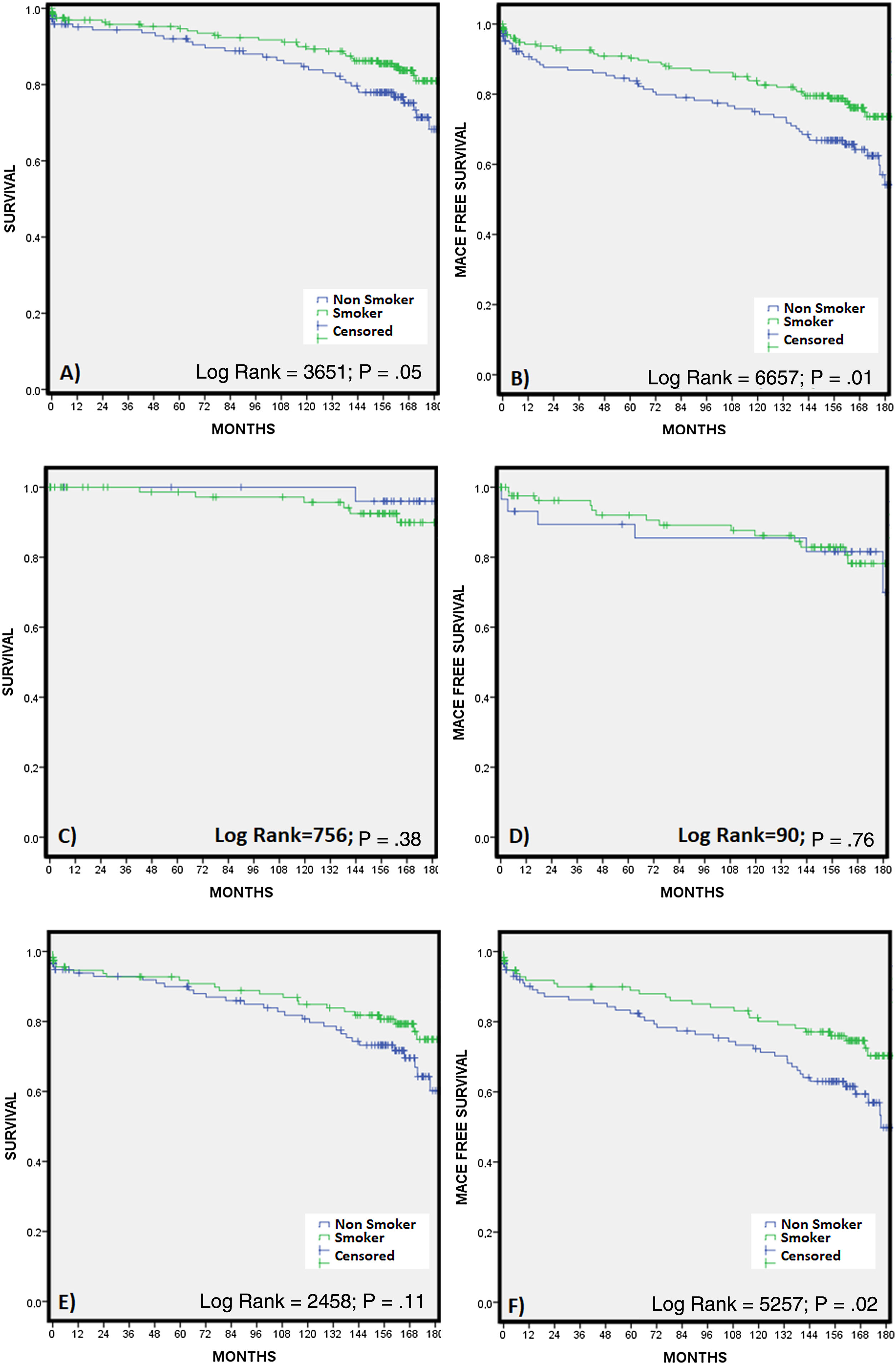
Long term follow-up and smoking habitThe median follow-up was 158.5 months [88.5–174.0]. Considering only the smokers, after discharge, 44.3% in the younger group, compared with the 55.7% in the senior cohort, maintained their smoking habit (P=.60). Over those, considering only patients alive at the final follow-up (n=159), these percentages rose up to 28.2% and 26.1%, respectively (P=.77). Fig. 3 shows through Kaplan–Meier curves the long-term outcomes stratified by the smoking habit of this cohort.
DiscussionThe present study reviews the so-called “smoking paradox” in young people. Although smoking seems more frequent in younger people, this cohort seemed to maintain the smoke paradox in the same way as in older patients. Excluding very old patients discards the strong influence of biological factors related to longevity, which could distort the effect of age adjusting. In fact, young patients with AMI had repeatedly been deemed to present a different clinical profile.17 Here, groups are paired by sex, so gender-related bias should disappear too. Similarly, diagnosis and admission date are matched by pairs, so we expect to discard any differences related to the tendency of applying the same management strategy. The smoking paradox has been repeatedly explained, among other theories, because non smokers were older. Our study shows that the smoker's paradox remains in the short-term after stratifying by age groups.
We further coincide with previous studies showing less short-term events in smokers and in younger patients when compared to non-smokers and veteran people. Our data shows that smokers presented less frequently hypertension and diabetes, higher left ventricular ejection fraction, less Killip degree at admission, a trend to showing better angiographic parameters (from epicardial flow-TIMI pre- and post-PCI-to myocardial perfusion–blush) and less PCI complications.1,2,5,6,9 This apparently “improved outcome” fits with the concept of the smoker's paradox in the past.
Our younger patients were more frequently smokers than the older. Consequently, smokers have been considered to present an acute myocardial infarction between 11 and 14 years before than non-smokers.6,9 However, our comparison stratified by age groups shows worse 30-day MACE rates in non-smokers compared with smokers, both among younger and older groups.
Smokers presenting an ST-segment elevation acute myocardial infarction are theoretically healthier and younger than non-smokers, with less diabetes, multivessel disease, etc. Thus, Andrikopoulos et al. analyzed a consecutive series of 7433 consecutive patients with ST-segment elevation acute myocardial infarction, and concluded that when we take into account the variables significantly related to output, including the age and gender, no favorable influence of habitual smoking on early outcome following acute myocardial infarction18 is observed. Similar influences of baseline characteristics have been reported by others.2,7,9,18–25 However, the influence of smoking on prognosis among 297 458 patients from the NRMI 2 study was only partially explained, changing the OR from 0.44 (95%CI, 0.43–0.45) to 0.86 (95%CI 0.83–0.89).6
In our study, when we included the angiographic parameters in the statistic model, the doubtful tobacco benefit decreased, pointing out a possible relationship between smoking and TIMI 3 pre- and post-PCI.23,26 Tobacco has been related to increased platelet activation, thrombus formation27–29 and endothelial disfunction.30–32
The smoker's paradox extends to other aspects of cardiovascular diseases, as heart failure or stroke, and the influence of other variables seems to explain the paradox. Abraham et al. suggest that smoking can precipitate hospitalization in patients with lesser underlying heart failure disease severity and as a result lower in-hospital mortality risk.4 Concerning the cerebrovascular disease, Ovbiagele et al. studied 2386 subjects, including 615 recent or current smokers and 1771 non-smokers. After adjusting for variables known to predict outcome after ischemic stroke, smokers had not only similar survival, but poorer functional outcomes than non-smokers.33 All these data point out a different mechanism in the infarction genesis. Smoker patients present more permeability-reperfusion in the coronary artery tree after treatment both after fibrinolysis7 and after PCI12,22,34 and less rates of reocclusion during follow-up.8,35 Some authors proposed the idea that smokers can have less damage to microvascular function,12 while others consider that the outcome differences are due to lower risk profile1,2,5 and faster epicardial flow,23 theories that agree with our findings.
In addition, Bliden et al. have also reported an increased platelet inhibition and lower aggregation in smoker patients on clopidogrel therapy.36 In our study, TIMI3 pre- and post-PCI modified the influence of smoking habit on prognosis. That suggests that some mechanism of the thrombotic occlusion may be different in young smokers than in older smokers. Perhaps they have a more transient trigger for thrombus formation, or the trigger is less permanent, so a successful angioplasty is easier and perhaps safer in them. In our study, no-reflow was more frequent in all non-smokers groups, which agrees with the reduced risk of re-occlusion found at 3 months in the APRICOT study.8
Furthermore, we should not lose sight of the fact that tobacco clearly does not improve the prognostic after a myocardial infarction. In fact, on one hand our follow-up data displays the lack of appropriate long-term smoking habit control, in concordance with several other studies, independently of age. On the other hand, with less statistic power due to smaller numbers, data depict the disappearance of the “tobacco benefit” in the young cohort (Fig. 3B).
Kaplan–Meier curves. (A) Global survival regarding smoking habit. (B) Major adverse cardiovascular events (MACE) free survival regarding smoking habit. (C) Young cohort survival regarding smoking habit. (D) Young cohort MACE-free survival regarding smoking habit. (E) Older cohort survival regarding smoking habit. (F) Older cohort MACE free survival regarding smoking habit.
Interestingly, Kievit et al. studied the effects of smoking on reocclusion and long-term cardiac outcome after successful fibrinolysis in 499 patients enrolled in the Antithrombotics in the Prevention of Reocclusion In Coronary Thrombolysis trials (APRICOT-1 and -2). Although 3-month reocclusion rate was lower in smokers, 5 year-survival and event-free survival was similar than in non-smokers.8 Outcomes after single percutaneous transluminal coronary angioplasty and coronary artery bypass grafting are better when tobacco cessation is achieved.20,37,38 Thus, smoking cessation significantly reduces long-term mortality, and counseling to quit smoking is an underused, very effective and costless intervention to improve long-term survival,39,40 even in older patients.41 In fact, Pell et al. reported that the number of admission for acute coronary syndrome decreased after implementing smoke-free legislation in the United Kingdom.42
Study limitationsIt must be considered that this was not a prospective randomized study. Data do not define cause and effect relationship and are mainly applied to male patients. Rather they identify associations between patient variables and follow-up events. The limited numbers could produce a lack of statistical capacity to detect relevant differences in some parameters. On the other hand, we did not differentiate among smokers, non-smokers and ex-smokers (recent, old, etc.). This together with the absence of registering some covariates that could affect the outcome (COPD, cancer, peripheral artery disease, stroke, family history, etc. could lead to a decrease of adjustment capacity in the multivariate model as a result of the above limitations.
ConclusionsSmokers were younger, had a lower risk profile, and a trend to have less short-term events than non-smokers. Although smoking was more frequent in the younger group, young smokers maintained the smoke paradox regarding short-term outcomes. Other cardiovascular risk factors in young people suffering an ST segment elevation myocardial infarction were more frequent in non-smokers as well. Despite a cardiac event, smoking habit frequently persist, independently of age, after long term follow-up. These findings can contribute to explain the apparently different course of myocardial infarction in young people and point out a different mechanism of infarction in smokers.
- -
In the short-term, smoker patients have been deemed to have better prognosis after an AMI.
- -
There are different explanations for the so-called “smoking paradox”. The main one is the different clinical profile between smoker and non-smoker AMI patients.
- -
One of the main differences reported in this clinical profile is age. Smoker patients clearly tend to be younger.
- -
Our aim was to assess the “smoking paradox” in young AMI patients and try to determine if it was maintained in this specific cohort, compared with an older group.
- -
Although smoking was more frequent in the younger group, young smokers maintained the smoke paradox regarding short-term outcomes, pointing out a different mechanism of infarction in smokers.
- -
Despite that, the smoking habit frequently persists, independently of age, after long term follow-up.
Abbreviations: MACE: major adverse cardiovascular events; MI: myocardial infarction; TIMI: Thrombolysis in Myocardial Infarction.