Global pandemics may affect the population in a wide variety of ways and everyone is at risk of its consequences. In Spain, since the beginning of the confinement due to the COVID-19 pandemic, a daily tribute to healthcare professionals is organized, as up to 15% of positive cases belong to this collective. Every day, at 8 pm, people go out to their windows and balconies to cheer-up and thank doctors, nurses, and the rest of healthcare professionals for their work and effort in this health crisis.
The first day that this tribute took place, a 63-year-old woman presented to the emergency department with chest pressure irradiated to both arms. She was clapping at the window, moved by the applause, accompanied by her family when the chest pain started. She did not present shortness of breath, palpitations, or syncope.
Her initial blood pressure was 154/96mmHg, her heart rate was 76beats/min, her respiratory rate was 15breaths/min and she had a saturation of 99% on room air. The physical examination, including the central nervous system examination, was unremarkable.
The patient did not have any cardiovascular risk factors. She was assessed 3 years ago because of exercise-related chest pain. A complete study was performed, including coronary angiography, and single-photon emission computed tomography with methoxy isobutyl isonitrile (SPECT-MIBI), without inducible ischemia or significant coronary stenosis. She did not take any medications.
The differential diagnosis was extensive in this previously healthy woman presenting with chest pain. It included acute coronary syndrome secondary to atherosclerotic disease, coronary vasospasm, microvascular angina, pericarditis, acute myocarditis, pulmonary embolism, and stress cardiomyopathy.
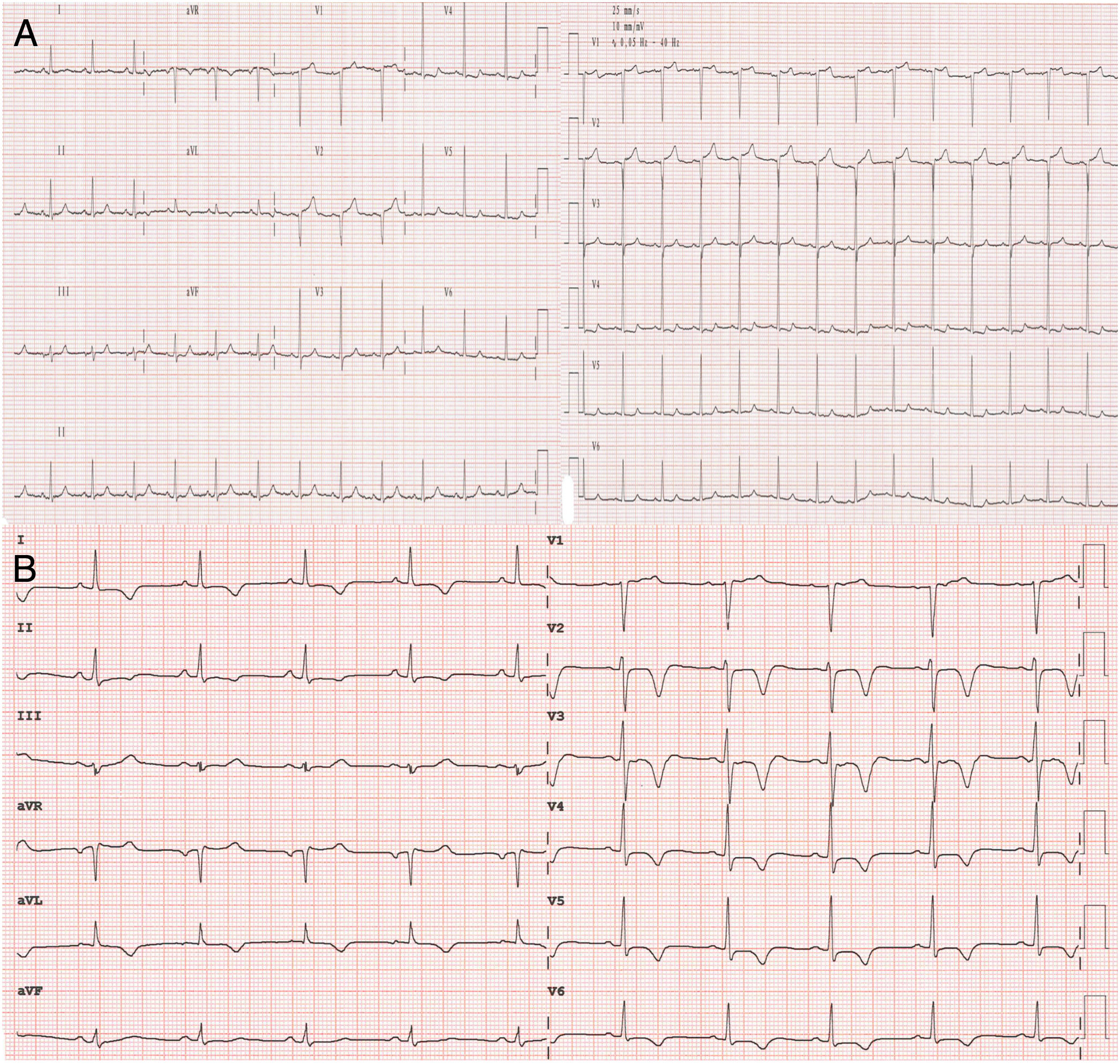
The first electrocardiogram (ECG), performed when the patient arrived, showed sinus rhythm with 1mm ST-segment depression in V4–V6 (Fig. 1A). Serial electrocardiograms after chest pain reduction showed correction of repolarization abnormalities. Her laboratory workup, including complete blood count, electrolytes, renal function, and N-terminal pro-brain natriuretic peptide levels, were normal. Cardiac biomarkers were elevated (troponin I 0.23–2.2–1.6; normal values < 0.01ng/mL).
The patient was initially treated as an acute coronary syndrome without ST elevation and was given treatment with aspirin, ticagrelor, fondaparinux, and atorvastatin.
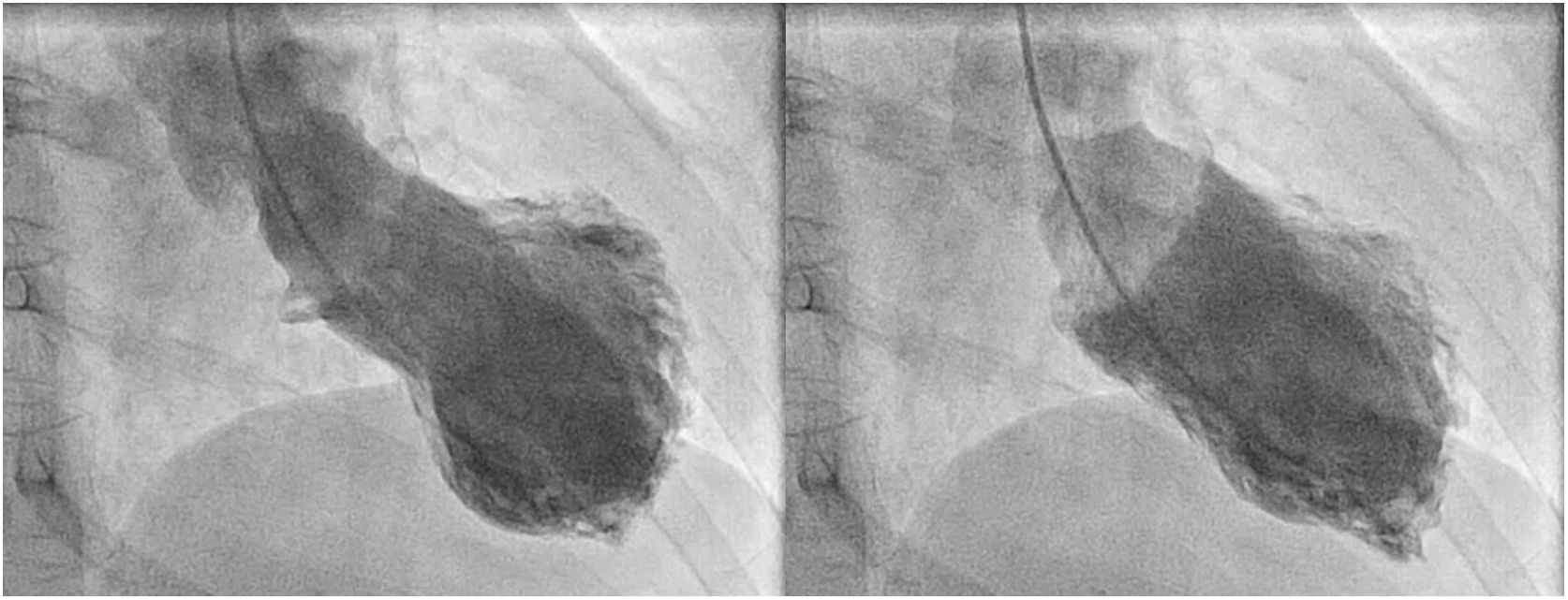
Bedside echocardiography demonstrated depressed left ventricular function with akinesia of the apical segments and mid anterior septum. The invasive coronary angiography, performed 24h after admission, showed mild stenosis in the left anterior descending artery. Left ventriculogram exhibited apical akinesia with hypercontractility of basal segments, and moderate left ventricular systolic dysfunction (Fig. 2) (video 1 of the supplementary data).
Taking into account all the previous findings, the case was interpreted as a typical variant of stress cardiomyopathy. Dual antiplatelet therapy and anticoagulation were withdrawn, and angiotensin-converting enzyme inhibitors and beta-blockers were started.
Repeat transthoracic echocardiogram performed 48h later, showed improvement of the left ventricular ejection fraction with an estimated left ventricular ejection function of 50%, with no evidence of systolic anterior motion of the mitral valve or outflow tract obstruction.
Serial electrocardiograms showed negative T waves in precordial leads and prolonged QTc interval (Fig. 1B), which progressively normalized in the following days, and the patient was discharged from hospital asymptomatic.
We present an unusual cause of acute stress-induced cardiomyopathy or tako-tsubo syndrome triggered by the collective acclaim of our population to the health care workers during the Spanish crisis.
Acute stress-induced cardiomyopathy is a cardiovascular entity that mimics acute coronary syndrome. This syndrome usually affects postmenopausal women, and it is frequently triggered by physical or emotional stress.1–3 It consists of transitory left ventricular systolic dysfunction in the context of normal coronary arteries.1–3 The pathophysiology is not completely understood, but it is thought that sympathetic hyperactivity due to an increase in circulating catecholamines leads to ventricular dysfunction.2,3 Several variants are described: the apical variant is the most common one and is more frequently associated with emotional triggers, whereas the midventricular and inverted types are less frequent, and are more commonly related with associated neurological damage.4,5
Since left ventricular function recovers in the following days or weeks after the beginning of symptoms, this syndrome was previously considered a benign entity with a very good prognosis. However, recent studies have demonstrated that the risk of mortality and complications in the acute phase of the disease is similar to that of acute coronary syndromes.3 The potential trigger involved in this pathology has been proved to be relevant regarding patients’ outcome, and elderly patients with emotional triggers have a lower risk than younger patients with physical triggers.
Tako-tsubo syndrome provoked by emotional triggers is usually associated with negative, traumatic, or stressful events. However, positive emotions can also trigger this syndrome in a small proportion of patients, which has been described as the “happy heart syndrome”,6 as in the herein case.
Repeat echocardiography performed 15 days after discharge demonstrated a complete recovery of left ventricular systolic function and wall motion abnormalities. The patient did not report new cardiovascular symptoms and continues clapping every evening during the COVID-19 quarantine.
Stress cardiomyopathy affects mainly middle-aged women and is frequently associated with emotional triggers. The daily touching tribute that takes place to acclaim health care professionals during the Spanish COVID-19 quarantine had in our case an unexpected cardiovascular consequence, as the heartwarming applause turned into a heartbreaking one.