Acute pulmonary embolism (PE) is the third most frequent acute cardiovascular syndrome. Systemic thrombolysis is the treatment of choice in patients with high-risk PE. The aim of this study is to analyze the patients diagnosed with pulmonary embolism at the emergency department, acute treatment decisions and the main outcomes.
MethodsA single-center retrospective observational study was conducted in patients with the diagnosis of PE at the emergency department over a period of 3 years, followed by a one-year period of follow-up. Reported P values below .05 indicate statistical significance.
ResultsA total of 240 patients presented the diagnosis of PE, with a mean age of 69.2 (± 17.4) years. Nearly a third of patients were classified with high or intermediate-high risk PE, but systemic thrombolysis was only performed in nine patients (3.8%). Among the high-risk PE subgroup, age (P=.06), gender (P=.54) and the existence of absolute and/or relative contraindications for thrombolysis (P=.99) were not predictors of the decision of non-revascularization. At the end of the follow-up period, 23.9% of the patients reported persisting symptoms, and chronic thromboembolic pulmonary hypertension was documented in 12.8% of the patients.
ConclusionsAcute treatment of pulmonary embolism is imperative to reduce mortality and prevent long-term sequelae. Systemic thrombolysis is the first line therapy in high-risk patients, but it is underused by medical population even in the absence of formal contraindications. It is necessary a new national-level model of actuation, implementing alternative strategies such as interventional ones to improve outcomes.
La embolia pulmonar (EP) aguda es el tercer síndrome cardiovascular agudo más frecuente. La trombolisis sistémica es el tratamiento de elección en los pacientes con EP de alto riesgo. El objetivo de este estudio es analizar los pacientes diagnosticados de EP en urgencias, las decisiones de tratamiento agudo y los principales resultados.
MétodosSe realizó un estudio observacional retrospectivo unicéntrico en pacientes con diagnóstico de EP en el servicio de urgencias durante un periodo de 3 años, seguido de un periodo de seguimiento de un año. Los valores de p inferiores a 0,05 indican significación estadística.
ResultadosUn total de 240 pacientes presentaron el diagnóstico de EP, con una edad media de 69,2 (± 17,4) años. Casi un tercio de los pacientes se clasificaron con EP de riesgo alto o intermedio/alto, pero solo se realizó trombolisis sistémica en 9 pacientes (3,8%). En el subgrupo de alto riesgo, la edad (p=0,06), el sexo (p=0,54) y la existencia de contraindicaciones absolutas o relativas para la trombolisis (p=0,99) no fueron factores predictivos de la decisión de no revascularización. Al final del periodo de seguimiento, el 23,9% de los pacientes refirieron síntomas persistentes, y se documentó hipertensión pulmonar tromboembólica crónica en el 12,8% de los pacientes.
ConclusionesEl tratamiento agudo de la embolia pulmonar es imprescindible para reducir la mortalidad y prevenir secuelas a largo plazo. La trombolisis sistémica es la terapia de primera línea en los pacientes de alto riesgo, pero está infrautilizada por la población médica incluso en ausencia de contraindicaciones formales. Es necesario un nuevo modelo de actuación a nivel nacional, implementando estrategias alternativas como las intervencionistas para mejorar los resultados.
Acute pulmonary embolism (PE), together with deep vein thrombosis are the entities of venous thromboembolism (VTE), the third most frequent acute cardiovascular syndrome, right after myocardial infarction and stroke.1 VTE incidence significantly increases with age, and it is increasing over time.2 The aging of populations and the increasing diagnostic capacity suggest that VTE will continue to play an important role in health care systems in the future.
In Portugal, the incidence of PE follows this trend and has also increased in recent years. Its estimated prevalence is 35 per 100,000 inhabitants, with women being more affected than men.3 Despite this increase in incidence, the in-hospital mortality has shown a positive evolution. This may be explained by two main factors: first, and the most important one, the improvement and greater effectiveness of hospital health care; secondly, the increase in diagnostic capacity, with an increasing amount of diagnosis of minor PE with low risk of mortality, and more accurate and early diagnosis allowing more efficient treatment.3
The diagnosis, risk assessment and treatment of patients with PE have been reviewed according to the latest studies and scientific evidence. The last European Society of Cardiology (ESC) guidelines focusing on the diagnosis and management of acute pulmonary embolism were published in 2019 and some concepts have been updated.4
Acute phase treatment includes hemodynamic and respiratory support, initial anticoagulation, and reperfusion treatment.4 Initial anticoagulation and reperfusion treatment are decided based on the assessment of pulmonary embolism severity.
Reperfusion therapy with systemic thrombolysis is the treatment of choice in patients with high-risk PE and the rescue therapy in patients who evolve to hemodynamic deterioration under anticoagulation treatment. Surgical embolectomy and percutaneous catheter-directed treatment (CDT) are recommended in patients whom thrombolysis is contraindicated or has failed. 4,5
The aim of this study is to analyze the main clinical characteristics of patients presenting to the emergency department with pulmonary embolism, acute treatment decisions and the main outcomes in-hospital mortality and incidence of long-term sequelae of pulmonary embolism.
MethodsA single-center retrospective observational study was conducted considering data from patients with the diagnosis of PE at the emergency department over a period of three years (from January 2016 to December 2018). Data regarding sociodemographic characteristics, medical background, clinical presentation, and therapeutic decisions were collected. Additionally, one-year follow-up was performed to evaluate long term outcomes. The research was carried out in accordance with internationally accepted recommendations for clinical investigation. According to SAGER guidelines, sex was defined as binary, designating the sex assigned at birth.
Statistical analysisCategorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions. Normal distribution was checked using Shapiro–Wilk test or skewness and kurtosis.
All reported P values are two-tailed, with a P value of .05 indicating statistical significance. Analyses were performed using software SPSS version 26.0 (IBM Corp, United States).
ResultsDemographics of the populationIn total, 240 patients aged 18 or over presented the diagnosis of PE during the defined period in our center. The mean age of the patients was 69.2 (± 17.4) years and 66.3% of PE episodes regarded female patients.
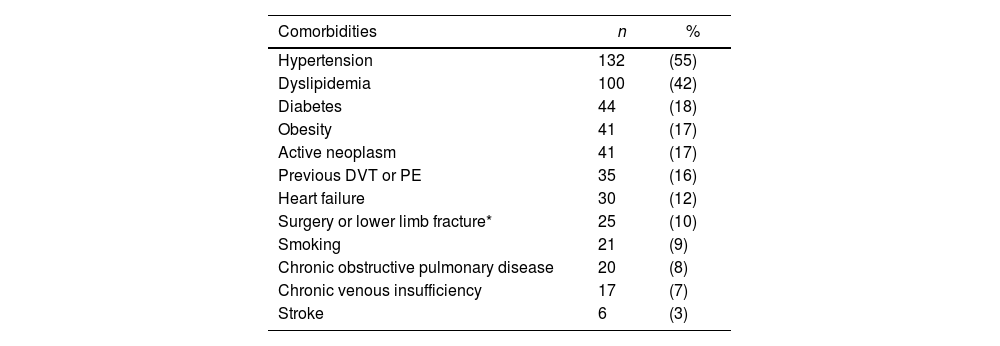
The most prevalent comorbidities among these patients were cardiovascular risk factors, with hypertension being the most expressive one (55%) and active neoplasm (17.1%) (Table 1).
Main comorbidities in patients with pulmonary embolism.
| Comorbidities | n | % |
|---|---|---|
| Hypertension | 132 | (55) |
| Dyslipidemia | 100 | (42) |
| Diabetes | 44 | (18) |
| Obesity | 41 | (17) |
| Active neoplasm | 41 | (17) |
| Previous DVT or PE | 35 | (16) |
| Heart failure | 30 | (12) |
| Surgery or lower limb fracture* | 25 | (10) |
| Smoking | 21 | (9) |
| Chronic obstructive pulmonary disease | 20 | (8) |
| Chronic venous insufficiency | 17 | (7) |
| Stroke | 6 | (3) |
When PE was suspected, the diagnostic work-up started based on clinical probability. All patients had imaging test for diagnosis, with computed tomography pulmonary angiogram (CTPA) being the most common choice (95.8% of the patients) due its availability in the emergency department.
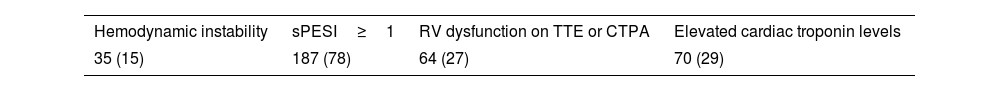
Clinical, imaging, and laboratory data were considered to classify the PE severity and stratify the risk of early death. The presence of hemodynamic instability was used to classify those with high-risk PE. For other clinical parameters of PE severity and/or comorbidity, we considered the simplified Pulmonary Embolism Severity Index (sPESI)≥1; the evidence of right ventricle (RV) dysfunction on CTPA or transthoracic echocardiogram; and elevated cardiac troponin levels. The presence or absence of these indicators allows the risk stratification of PE in high, intermediate-high, intermediate-low, or low, accordingly to the ESC guidelines for management of acute PE.
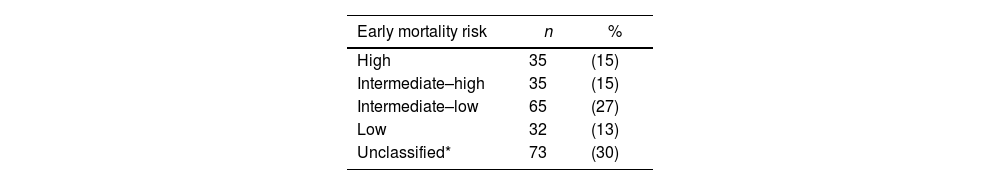
Most of the patients presented intermediate-low or low risk PE, but nearly a third of them (29.2%) were classified with high-risk or intermediate-high risk PE (Table 2). The prevalence of each individual indicator of risk in this population is shown in Table 3.
Risk stratification of patients with pulmonary embolism.
| Early mortality risk | n | % |
|---|---|---|
| High | 35 | (15) |
| Intermediate–high | 35 | (15) |
| Intermediate–low | 65 | (27) |
| Low | 32 | (13) |
| Unclassified* | 73 | (30) |
Indicators of risk in patients with pulmonary embolism.
| Hemodynamic instability | sPESI≥1 | RV dysfunction on TTE or CTPA | Elevated cardiac troponin levels |
|---|---|---|---|
| 35 (15) | 187 (78) | 64 (27) | 70 (29) |
CTPA, computed tomography pulmonary angiogram; sPESI, simplified pulmonary embolism severity index; TTE, transthoracic echocardiogram.
Data are expressed as no. (%).
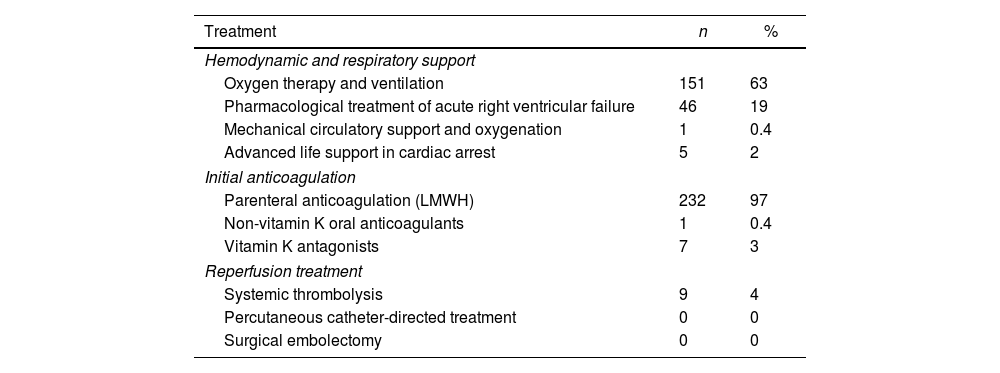
The first step in the treatment of patients presenting with PE is to guarantee hemodynamic and respiratory support whenever needed. Respiratory failure was common and nearly 63% of the patients needed oxygen therapy and/or ventilation. Mechanical circulatory support was performed in only 1 patient after transfer to another hospital. A total of 5 (2.1%) patients presented with cardiac arrest; 3 of them were successfully treated with systemic thrombolysis.
All patients early started on anticoagulation, most of them with weight-adjusted low-molecular weight heparin (96.7%).
Reperfusion treatment was performed in nine patients (3.8%), with systemic thrombolysis being the treatment of choice, representing 25.7% of the patients with high-risk PE.
Percutaneous catheter-directed treatment and surgical embolectomy are not available in our center and were not performed (Table 4).
Acute-phase treatment of patients with pulmonary embolism.
| Treatment | n | % |
|---|---|---|
| Hemodynamic and respiratory support | ||
| Oxygen therapy and ventilation | 151 | 63 |
| Pharmacological treatment of acute right ventricular failure | 46 | 19 |
| Mechanical circulatory support and oxygenation | 1 | 0.4 |
| Advanced life support in cardiac arrest | 5 | 2 |
| Initial anticoagulation | ||
| Parenteral anticoagulation (LMWH) | 232 | 97 |
| Non-vitamin K oral anticoagulants | 1 | 0.4 |
| Vitamin K antagonists | 7 | 3 |
| Reperfusion treatment | ||
| Systemic thrombolysis | 9 | 4 |
| Percutaneous catheter-directed treatment | 0 | 0 |
| Surgical embolectomy | 0 | 0 |
LMWH, low-molecular-weight heparin.
When analyzing the high-risk PE subgroup, we verified that age (72.6±16.1 vs 64.0±5.9; P=.06), gender (P=.54), and the existence of absolute and/or relative contraindications for thrombolysis (P=.99) were not predictors of the decision of non-revascularization as we initially expected.
In-hospital mortalityThe in-hospital mortality rate was 9.6% (n=23) with 60.9% of deaths occurring in males. The average age of deceased patients was 76.9 years, higher than surviving patients with 68.3 years (P<.05). The average time from admission to death was 10.5 (± 7.8) days. Of these patients, 39.1% had an active neoplasm and at least 34.7% of them already showed signs of RV disfunction on echocardiogram at admission.
Of these patients, 11 (47.8%) presented high (n=4) or intermediate-high risk PE (n=7) on admission. This represents a mortality rate of 11.4% among high-risk patients and 20% among intermediate-high risk PE patients, significantly higher than 5.2% among low or intermediate-low risk PE patients.
Long-term sequelaeFollow-up data up to December 2020 were analyzed to better characterize possible long-term sequelae of pulmonary embolism. A total of 29 patients (12.1%) died during this period of follow-up. Since data about the circumstances of these deaths are not available, in this analysis are consider the remained 188 patients.
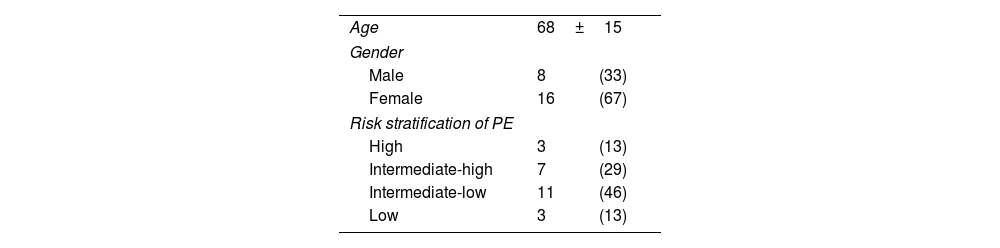
In December 2020, 45 patients (23.9%) reported persisting symptoms and functional limitation since the event. Chronic thromboembolic pulmonary hypertension was documented in 24 patients (12.8%) (Table 5), and 10 patients (5.3%) had recurrence of VTE, all of them under effective anticoagulation.
Characteristics of patients diagnosed with chronic thromboembolic pulmonary hypertension at follow-up (n=24).
| Age | 68±15 | |
| Gender | ||
| Male | 8 | (33) |
| Female | 16 | (67) |
| Risk stratification of PE | ||
| High | 3 | (13) |
| Intermediate-high | 7 | (29) |
| Intermediate-low | 11 | (46) |
| Low | 3 | (13) |
PE, pulmonary embolism.
Data are expressed as no. (%) or mean±standard deviation.
Despite the current recommendations, only 25.7% of high-risk PE patients were managed with systemic thrombolytic therapy in our center. Among the 35 patients with intermediate-high risk PE, all were on anticoagulation with no further therapeutic interventions, even those with clinical deterioration and death. When analyzing the reasons for these therapeutic decisions, 2 of the patients had suffered an ischemic stroke in previous 6 months (an absolute contraindication for systemic thrombolysis; 1 patient had advanced liver disease and 2 patients were on oral anticoagulation) relative contraindications. The remaining patients had no formal contraindication to the procedure.
The reluctance to use thrombolytic therapy even in the absence of contraindications might be explained by a perceived increased risk of bleeding in patients with active malignancies, advanced age, or multiple comorbidities.6 Although we found no predictors of non-revascularization in our population, this may be explained by the small number of patients undergoing systemic thrombolytic.
Some recent studies have proposed the percutaneous CDT as an alternative to thrombolysis in patients with a perceived increased risk of bleeding, showing minimal major bleeding and improvement in right ventricular function by relieving the thromboembolic obstruction.7–11
The high mortality rate among patients with in intermediate-high risk PE shows how the management of these patients can be challenging since they present normal hemodynamics at initial evaluation. After initial treatment, it might be difficult to identify signs of treatment failure and redefine a new strategy. Studies have shown that even patients with no signs of RV disfunction and normotensive at first evaluation may deteriorate after the beginning of the treatment.11–14 This enhances the need to properly evaluate patients in this category of risk and early select those who might benefit from fibrinolytic therapy preventing hemodynamic deterioration without an increase in the risk of major hemorrhagic event.15
The definition of the best management strategy in patients with several comorbidities or with clinical deterioration may be challenging and must be individualized. Furthermore, it is not completely clear how to define a “treatment failure” and when to move on to another therapeutic approach. Since no evidence alone is enough to support these decisions, current guidelines recommend deciding based on the expert knowledge of a multidisciplinary team, in the form of Pulmonary Embolism Response Team (PERT), especially the management of high and intermediate-high risk PE when uncertainties remain regarding the best approach.13,16 This multidisciplinary team might help to define the best strategy based on individual characteristics of the patient and local expertise (Fig. 1).
Defining the optimal approach enhances the likelihood of success in the acute phase and reduces the risk of long-term sequelae, being the most clinically relevant being the chronic thromboembolic pulmonary disease with or without pulmonary hypertension, resulting from vascular remodeling and/or incomplete resolution of pulmonary thrombi. In our study, the cumulative prevalence of chronic thromboembolic pulmonary disease over four years was 34.8%, as expected by the literature, with values of chronic thromboembolic pulmonary hypertension of 12.8%, a noteworthy number.17–19 Although this could stem from the limited use of more aggressive therapies within high or intermediate-high risk subgroups of patients, most of these patients cluster within the intermediate-low risk category. When analyzing these patients, it was observed that three of them had previously experienced thromboembolic events, suggesting the plausibility of an acute-on-chronic event instead of isolated acute event. Furthermore, seven patients presented with chronic heart failure, and four with active cancer, both conditions predisposing to VTE, often with subclinical manifestations.
Patients with chronic thromboembolic pulmonary hypertension were seldom referred for specialized centers, remaining without proper treatment. Of the few who were referred, 2 underwent balloon pulmonary angioplasty, yielding favorable outcomes in symptom management. Unfortunately, additional data is not available as these patients are subsequently followed up at another institution to which we lack access. To our knowledge, none of the patients underwent pulmonary endarterectomy.
Patients who survived the first 30 days after PE seem to present higher mortality than expected in the general population, being the active cancer at the time of PE the most important predictor of mortality.17,20
Although data regarding the causes of death during the follow-up period are not available, 12 (41.4%) of these patients had active neoplasms and 7 of them (24.1%) had dementia at the time of PE, comorbidities that significantly increase the patient's frailty and risk ok death.
Strengths and limitationsData on epidemiology, management and outcomes of PE in Portugal is scarce. With this work we detail the clinical approach of PE in a major Portuguese single center, highlighting the need to improve and update our current practice regarding the PE.
Limitations of this study include its retrospective nature, small sample size. The retrospective nature of our study limited the ability to understand the reason of some therapeutic decisions. Some medical record had insufficient clinical information for risk stratification. Frequently, the cardiac troponin levels were not measured, and echocardiogram was not performed at the time of diagnosis. This lack of data may impact the severity classification, with more patients being wrongly classified with low-risk events with consequences in therapeutic approach and clinical outcomes.
ConclusionsAcute treatment of pulmonary embolism is imperative to reduce mortality and prevent long-term sequelae. Systemic thrombolysis is the first line therapy in high-risk patients, but it is underused by medical population even in the absence of formal contraindications.
This data suggests that is necessary a new national-level model of actuation, implementing alternative strategies such as interventional ones to improve outcomes.
Reperfusion therapy with systemic thrombolysis is the treatment of choice in patients with high-risk PE. The main concerns about systemic thrombolysis are related to the increased risk of bleeding. For this reason, only a small number of unstable patients undergo thrombolysis in clinical practice. In this context, the use of percutaneous CDT for the treatment of acute PE has emerging over the past years. Multidisciplinary pulmonary embolism response teams (PERT) is a concept developed for the management of high-risk and selected cases of intermediate risk PE to standardize and improve the care of these patients.
What does this study add?This study adds data on epidemiology, management and outcomes of PE in a Portuguese center, since data are scarce. Reperfusion treatment was substantially underused in high-risk PE. Although the main concern with thrombolysis is the risk of bleeding, in this study age, gender and the existence of absolute and/or relative contraindications for thrombolysis were not predictors of the decision. A significant percentage of patients (24%) reported persisting symptoms and functional limitation one year after the event.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerationsThe work was approved by the Ethics Committee of the Hospital of Braga. Patient's informed consented does not apply to this work. We confirm that the possible variables of sex and gender have been taken into account in accordance with the SAGER guidelines.
Statement on the use of artificial intelligenceArtificial intelligence was not used in the development of this work.
Authors’ contributionsM. Dias was responsible for the conception of the work, as well as the acquisition, analysis, and interpretation of data, and drafting the work. R. Silva, F. Ribeiro Mané, I. Conde, and S. Fernandes were responsible for the acquisition and analysis of data, as well as drafting the work. C. Ferreira, F. Vilela, and O. Pires acquired and analyzed data for the work and drafted the manuscript. Ferreira, F. Vilela, and O. Pires acquired and analyzed data for the work and drafted the manuscript. N. Salomé analyzed and interpreted the data and revised the manuscript for important intellectual content. All authors meet all the characteristics defined by the International Committee of Medical Journal Editors in the criteria for authorship of scientific articles.
Conflicts of interestNone declared.
Abbreviations: CDT: catheter-directed treatment; PE: pulmonary embolism; PERT: pulmonary embolism response teams; RV: right ventricle.