Vasovagal syncope (also known as neurocardiogenic syncope) is the most common cause of syncope.1 Vasovagal syncope may result in physical injury, psychological distress, including anxiety and depression, and impairment of quality of life.2,3 Current management of vasovagal syncope is challenging and includes non-pharmacological approaches (i.e. orthostatic training), pharmacological treatment (i.e. midodrine, fludrocortisone or beta-blockers) and more recently closed-loop stimulation or cardio-neuro ablation. However, most of them have limited efficacy2,3 and new therapeutic strategies are warranted.
Vasovagal syncope results from a complex neurologic reflex, in which dysfunction of the autonomic nervous system, particularly the response of the sympathetic system and the baroreflex, plays a key role. In fact, syncope is preceded by sinus tachycardia at tilt test evaluation in most patients with vasovagal syncope.3,4 In addition, previous studies have suggested that beta-blockers reduce the excessive release of catecholamines which may promote the hypotensive response, leading to syncope. However, studies assessing the effects of beta-blockers in preventing vasovagal syncope have provided mixed results, likely due to concomitant hypotensive effects of these drugs.5
In this clinical setting, treatments that modulate these aspects may be helpful to reduce the risk of recurrence. Ivabradine is an I(f) current blocker that slows heart rate, without a substantial impact on blood pressure. In addition, it has been suggested that ivabradine could potentially reduce the release of catecholamines, without a concomitant hypotensive effect. Furthermore, ivabradine has been shown to have some efficacy in the treatment of postural orthostatic tachycardia syndrome, as well as in patients with inappropriate sinus tachycardia.6 We speculate that treatment with ivabradine may improve recurrent syncope in patients with vasovagal syncope.
This was a real-life study performed according to local clinical practice. We present a case series of 20 patients treated with ivabradine 5–7.5mg twice a day (target dose according to baseline heart rate) for recurrent vasovagal syncope despite guideline-recommended treatment. Another patient with vasovagal syncope was excluded from the analysis as ivabradine was not tolerated due to symptomatic bradycardia. Complete response was defined as the absence of recurrence of syncope after initiation of treatment with ivabradine and partial response as the reduction in the number of episodes. The study was conducted in accordance with the Declaration of Helsinki. All patients gave their informed consent for this study.
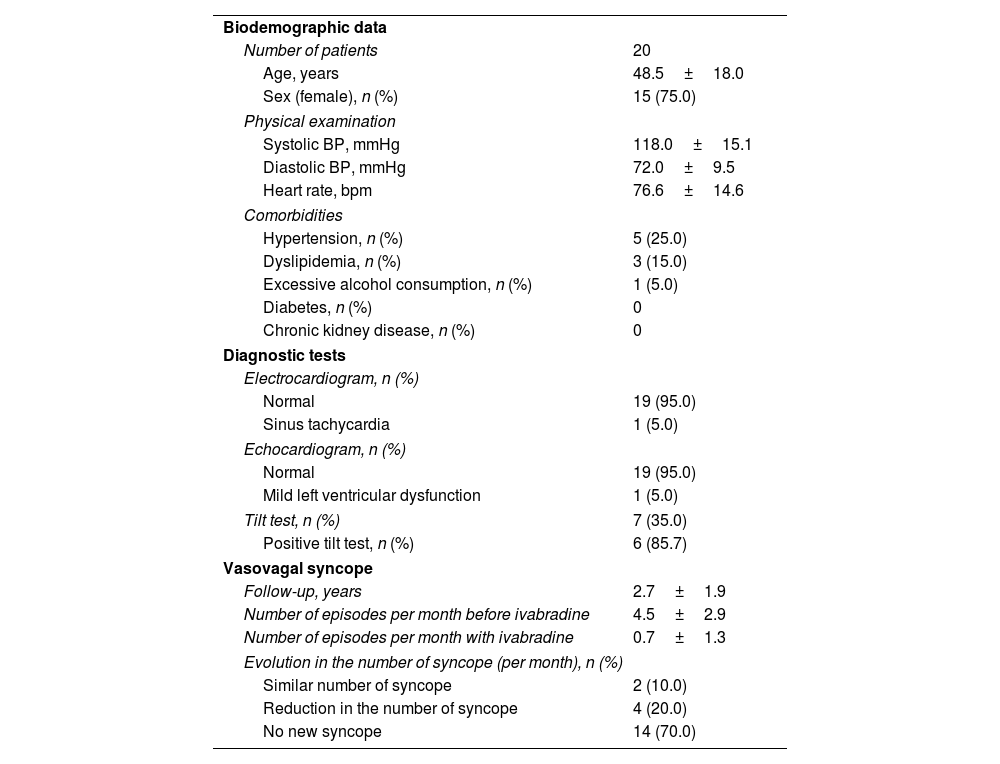
Mean age was 48.5±18.0 years, 75.0% of patients were women, 25.0% had hypertension and 95.0% had a normal echocardiogram and an electrocardiogram. Only one patient had mild left ventricular dysfunction and another one had basal sinus tachycardia. Seven (35.0%) patients underwent a tilt test before being treated with ivabradine which confirmed the diagnosis of vasovagal syncope in 85.7% of cases.
After a mean follow-up of 2.7±1.9 years, the mean number of episodes per month decreased from 4.5±2.9 to 0.7±1.3 (P<.01). 90% of patients obtained partial (4 [20%]) or complete (14 [70%]) response to ivabradine. Ivabradine did not have any effect in only two patients. In patients with a complete response to ivabradine, the number of episodes of syncope per month decreased from 4.7±3.4 to 0, in those with partial response from 4.0±1.4 to 1.25±0.5 and in those without any response, the number of episodes remained in 4.0±1 (Table 1). In the six patients with a positive tilt test in which sinus tachycardia before collapse was observed, a partial or complete response to ivabradine was observed. In the patient with a negative tilt test, a partial response to ivabradine was shown. There were no side effects associated with ivabradine.
Clinical and follow-up data from vasovagal syncope patients treated with ivabradine.
| Biodemographic data | |
| Number of patients | 20 |
| Age, years | 48.5±18.0 |
| Sex (female), n (%) | 15 (75.0) |
| Physical examination | |
| Systolic BP, mmHg | 118.0±15.1 |
| Diastolic BP, mmHg | 72.0±9.5 |
| Heart rate, bpm | 76.6±14.6 |
| Comorbidities | |
| Hypertension, n (%) | 5 (25.0) |
| Dyslipidemia, n (%) | 3 (15.0) |
| Excessive alcohol consumption, n (%) | 1 (5.0) |
| Diabetes, n (%) | 0 |
| Chronic kidney disease, n (%) | 0 |
| Diagnostic tests | |
| Electrocardiogram, n (%) | |
| Normal | 19 (95.0) |
| Sinus tachycardia | 1 (5.0) |
| Echocardiogram, n (%) | |
| Normal | 19 (95.0) |
| Mild left ventricular dysfunction | 1 (5.0) |
| Tilt test, n (%) | 7 (35.0) |
| Positive tilt test, n (%) | 6 (85.7) |
| Vasovagal syncope | |
| Follow-up, years | 2.7±1.9 |
| Number of episodes per month before ivabradine | 4.5±2.9 |
| Number of episodes per month with ivabradine | 0.7±1.3 |
| Evolution in the number of syncope (per month), n (%) | |
| Similar number of syncope | 2 (10.0) |
| Reduction in the number of syncope | 4 (20.0) |
| No new syncope | 14 (70.0) |
BP: blood pressure; bpm: bytes per minute.
In our study, 90% of patients had complete or partial abolishment of recurrent syncope at follow-up under ivabradine therapy. This may be explained by a reduction in catecholamines release in those cases that presented with sinus tachycardia preceding syncope, as it has been previously hypothesized.5 A study by Sutton et al. of 25 patients with sinus tachycardia before collapse on tilt test showed that after a mean follow-up of 15 months, 5 patients did not show any change, 10 patients improved and 8 patients had no recurrent symptoms at follow-up. This represents a partial or complete response in 72% of patients with ivabradine. In addition, only one patient required drug discontinuation due to side effects.6 All these data indicate that ivabradine could be useful for the treatment of some patients with vasovagal syncope. The benefits of ivabradine in these patients could be explained due to its effects in reducing the response of the sympathetic system that occurs during some types of vasovagal syncope.4 Thus, ivabradine would be useful in those patients that present with sinus tachycardia before collapse on tilt testing.
In addition, ivabradine is a well-tolerated drug, with a low-risk of side effects in contrast to other drugs used for vasovagal syncope, such as midodrine or beta-blockers.1–3 This is important given that many patients with vasovagal syncope are young women with normal or low blood pressure which could be further lowered by beta-blockers, resulting in drug intolerance or symptomatic hypotension.1–3 As ivabradine is better tolerated, a full use of this drug could be anticipated and higher response may be expected. This is supported by our study since 90% of patients reported a marked benefit or complete resolution of symptoms. As a result, in patients with recurrent vasovagal syncope, treatment with ivabradine could be attempted, except in those cases with bradycardia, even when a confirmatory tilt test cannot be not performed.
Our study presents several limitations. First, the results were not compared with a control group and therefore should be considered hypothesis generating until validation by a controlled randomized trial. Secondly, a tilt test was not performed in all patients. However, diagnosis of vasovagal syncope is done with the clinical presentation and exclusion of other syncope causes and does not need to be confirmed with tilt testing. In any case, our results should be confirmed by a controlled randomized trial.
In conclusion, and despite these limitations, the low efficacy of other drugs and the safety profile of ivabradine support a trial attempt with it in recurrent vasovagal syncope patients, except if they present with bradycardia prior to syncope.
FundingNo funding was obtained for this study.
Ethical considerationsThis study was conducted in accordance with current ethics guidelines, and was approved by the Ethics Committee of our center (Hospital Universitario La Paz). The study was conducted in accordance with the Declaration of Helsinki. All patients gave the informed consent for this study. Possible variables of sex and gender have been considered in accordance with the SAGER guidelines in this work. Study reporting followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Statement on the use of artificial intelligenceNo artificial intelligence tool was used in the development of this work.
Authors’ contributionsAll authors were involved in the design, data gathering, result interpretation, preparation, and approval of the article.
Conflicts of interestAuthors do not have any conflict of interest regarding this manuscript.