The pocket sized KardiaMobile (KM) is a monitoring device for ECG recording through a smartphone-based application. This system is generally aimed as screening tool to detect alterations in cardiac rhythm but its diagnostic potential for detection of ST changes remains largely unknown. This study sought to assess the diagnostic sensitivity of the KM system for detection of ST changes in patients with ST elevated myocardial infarction (STEMI).
MethodsPatients admitted with diagnosis of STEMI were consecutively included. Recordings with KM were obtained in leads I, II and anterior precordial. KM recordings were obtained as well from healthy individuals. All recordings were submitted for blinded assessment.
ResultsA total of 112 patients with STEMI and 25 healthy individuals were included. Among those showing ST changes, these consisted mostly in depression (75%). Sensitivity was modest for individual leads (57-58%). The combination of 2-leads, when including the precordial, and the combination of 3-leads markedly increased sensitivity (88-98% and 100% respectively) for both inferior and anterior STEMI. Specificity was very high (96-100%) and the Youden's J statistic was excellent for the 2-leads combinations that included the precordial lead (0.84-0.94) and for the 3-leads combination (0.96).
ConclusionsThe Kardia Mobile system with the combination of 2-leads (I+precordial or II+precordial) or 3-leads shows a very high sensitivity for both anterior and inferior STEMI.
El KardiaMobile (KM) es un dispositivo portátil que permite el registro de una derivación electrocardiográfica a través de una aplicación para telefonía móvil. Este sistema se usa generalmente como cribado en la detección de arritmias, pero su potencial diagnóstico para la detección de cambios del segmento ST es en gran medida desconocido. Este estudio buscó evaluar la sensibilidad diagnóstica del sistema KM para la detección de cambios del segmento ST en pacientes con infarto de miocardio con elevación del segmento ST (IAMCEST).
MétodosSe incluyó una serie consecutiva de pacientes ingresados con diagnóstico de IAMCEST. Se obtuvieron registros con KM en las derivaciones I, II y precordial anterior. También se obtuvieron registros por KM de individuos sanos. Todos los registros se enviaron para evaluación cegada.
ResultadosSe incluyó a 112 pacientes con IAMCEST y a 25 individuos sanos. Entre los que mostraron cambios del segmento ST estos consistieron, principalmente, en depresión (75%). La sensibilidad fue pequeña para las derivaciones individuales (57-58%). La combinación de dos derivaciones, incluida la precordial, y la combinación de tres derivaciones aumentaron notablemente la sensibilidad (88-98% y 100% respectivamente) en el IAMCEST inferior y anterior. La especificidad fue muy alta (96-100%) y el estadístico J de Youden fue excelente para las combinaciones de dos derivaciones que incluyeron la derivación precordial (0,84-0,94) y para la combinación de tres derivaciones (0,96).
ConclusionesEl sistema KardiaMobile con la combinación de dos derivaciones (I más precordial o II más precordial) o tres derivaciones muestra una sensibilidad muy alta para IAMCEST anterior e inferior.
ST elevated myocardial infarction (STEMI) remains nowadays a serious health condition. These patients require immediate reperfusion treatment and the earlier its application the higher the clinical benefit derived. Nonetheless, patients take several hours to make the decision to seek medical care.1–3 This is a critical issue since the mortality of STEMI concentrates in the prehospital setting within the first 2hours and because the reperfusion therapies provide a lower benefit as becoming less timely applied.
Nowadays, smartphones have become part of our life and have enabled several ways of cardiovascular monitoring; cardiac rhythm monitoring in particular has experienced one of the highest growths in recent years. Starting with pulse detection to the electrocardiographic recordings, several wireless devices have demonstrated their suitability for hearth rhythm monitoring.4–8 The pocket sized KardiaMobile 1L (AliveCor, United States) is a monitoring device that requires the patient to trigger the electrocardiogram (ECG) recording. (Fig. 1) This handheld technology involves the use of a pair of electrodes linked to a mobile device to provide a single-lead rhythm strip. The device was initially developed to detect atrial fibrillation.9,10
Among all these systems only the AliveCor Heart Monitor (AliveCor, United States) has been evaluated in small series of patients with STEMI.11,12 However, given its technical characteristics and mode of use, this system is designed to be used by healthcare/emergency professionals at extrahospital points of care. Anecdotal experiences have been reported showing ischemic changes in 2 patients while using wearable systems like the Apple Watch (Apple Inc., United States).13
The KardiaMobile 1L ECG system has not been evaluated in the detection of ST-T changes related with ischemia. Our aim was to show how 1-lead, 2-leads, and 3-leads equivalent ECG by using KardiaMobile 1L have the potential ability of distinguishing changes on ST segment in patients with ST elevated myocardial infarction.
MethodsThis is a prospective study conducted in a single center that included consecutive patients with a confirmed diagnosis of STEMI, based on the universal definition of myocardial infarction criteria.14 Accordingly, patients had to meet the following electrocardiographic criteria for ST segment elevation: new ST-elevation at the J-point in 2 contiguous leads with the cut-point ≥ 1mm in all leads other than V2–V3 leads where the following cut-points apply: ≥ 2mm in men ≥ 40 years; ≥ 2.5mm in men<40 years, or ≥ 1.5mm in women regardless of age.
Unconscious or intubated patients, those presenting after cardiac arrest, patients with cardiogenic shock and those who showed a high degree of emotional involvement or considered unsuitable for consenting were excluded. Finally, patients in whom participation could imply a delay in reperfusion treatment were also excluded. The latter refers to those cases in which obtaining KM recordings could defer the immediate transfer to the cath lab.
In addition, 25 healthy individuals showing strictly normal conventional 12-leads electrocardiography recordings were recruited. Individuals showing early repolarization or bundle branch blocks were excluded. The study was basically aimed to assess sensitivity of the system for ST changes during STEMI, the evaluation of specificity was a secondary endpoint focused as a first stage in normal ECG recordings.
The study was approved by the Institutional Review Board of the institution. A specific informed consent was obtained in all patients included in this study.
ProceduresPatients who met all criteria were offered participation, which did not entail any delay in the application of precise care measures, specifically reperfusion with primary angioplasty, which is the method of systematic reperfusion in our region. The KardiaMobile (KM) ECG recordings were obtained immediately during the time period elapsed between the activation of the infarction code and the performance of primary angioplasty. In addition, KM ECG recordings were collected from the 25 healthy individuals showing strictly normal conventional 12-leads electrocardiography recordings.
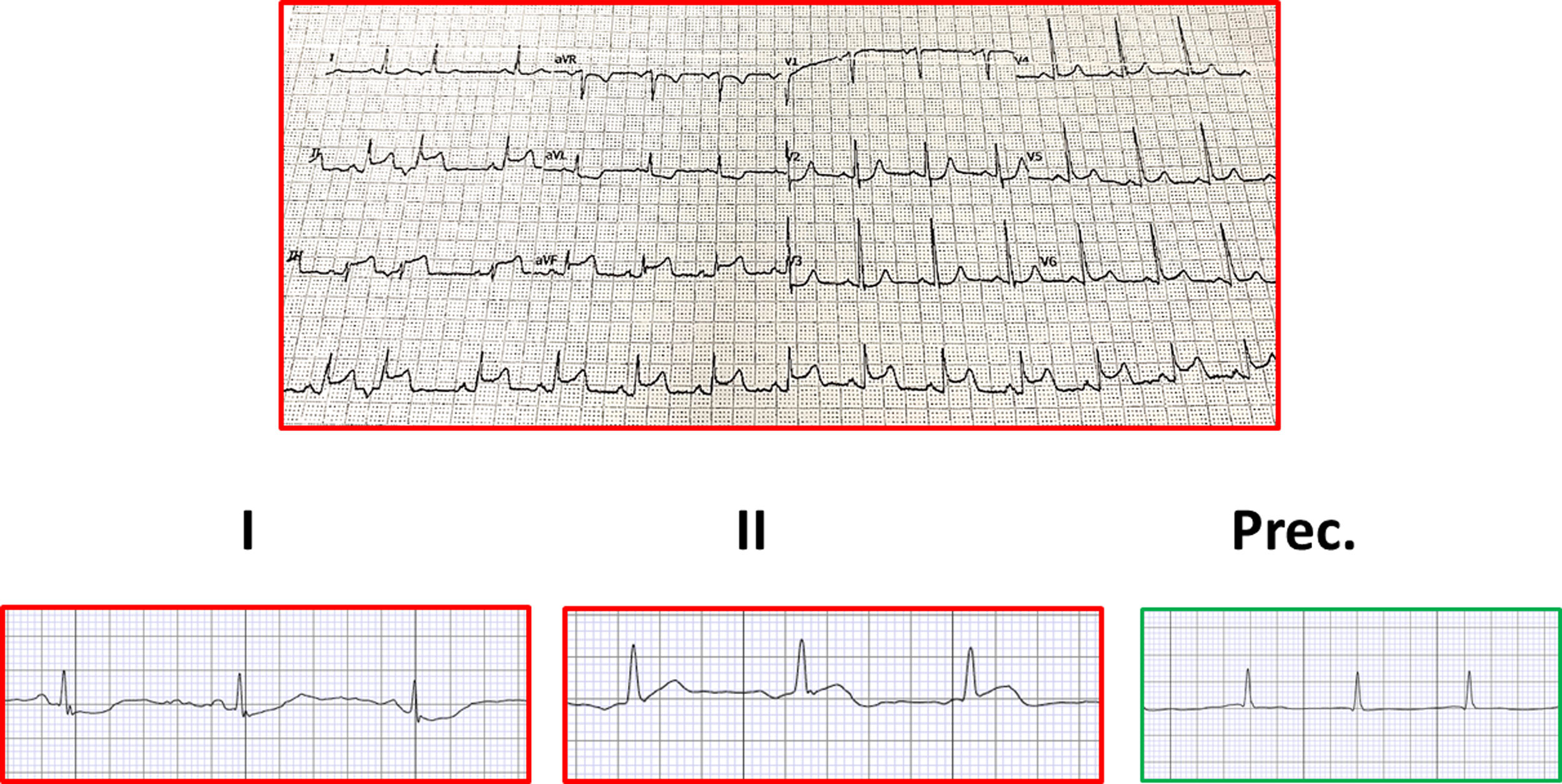
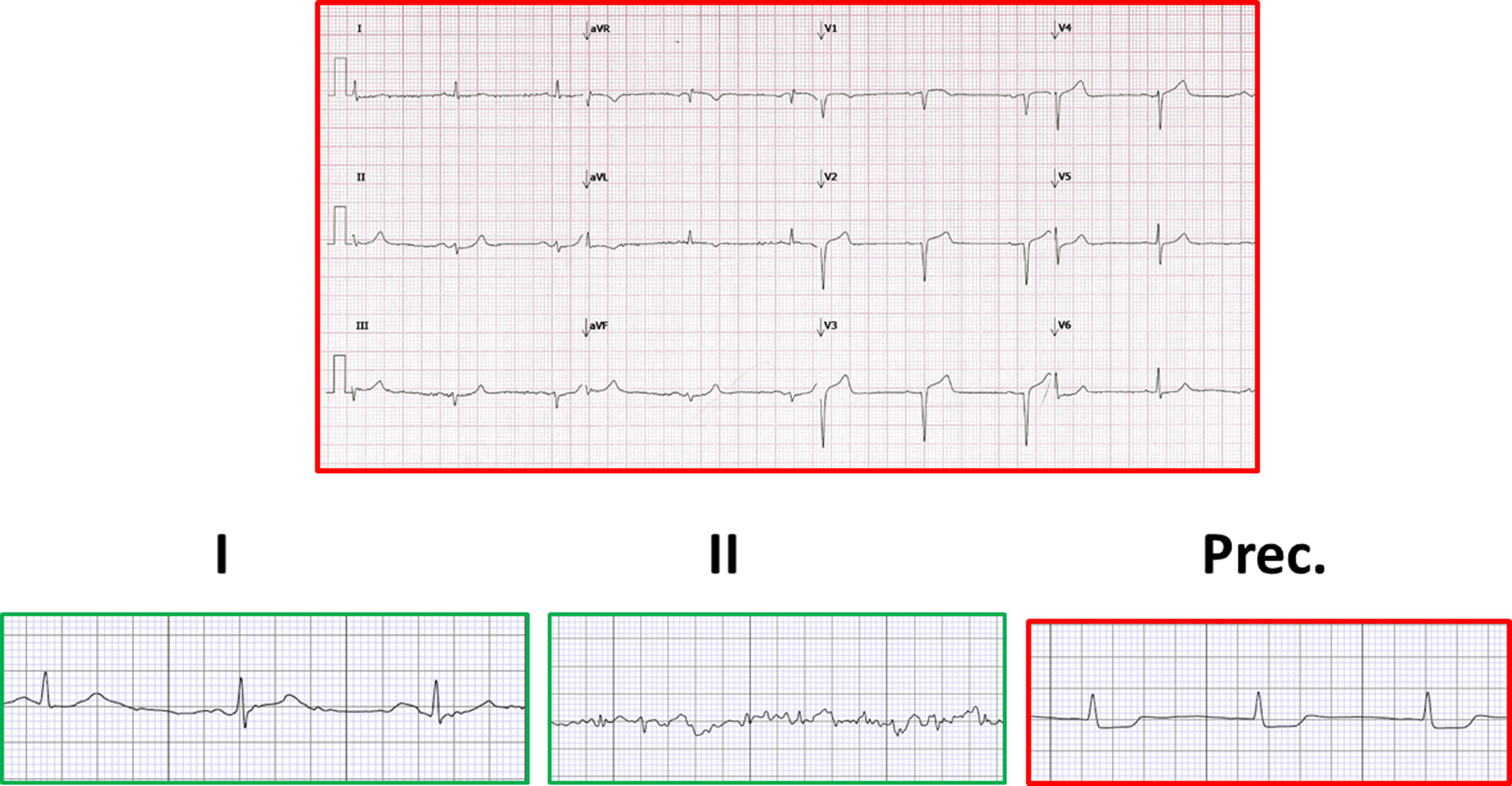
KM ECG readings were obtained in lead I (placing sensors on the fingers of both hands), lead II (placing sensors on the right hand fingers and left knee) and anterior precordial lead (Fig. 2). The investigators were previously trained by personnel linked to the system commercialization. The recordings were sent to a mail-box of the principal investigator. The records were then ungrouped (mixing STEMI and healthy), anonymized and number-coded. After these procedures the recordings were sent to a 2 blinded cardiologists not directly involved in the study execution.
The criteria for considering ST segment elevation or depression in the KM ECG recording was the observation of a ST shift with respect to point J of more than 1mm. In cases of discrepancy between the 2 blinded investigators, consensus was reached after consulting a third party.
StatisticsData values for patients characteristics are presented as n (%), mean±standard deviation or median (interquartile range) as required. Sensitivity and specificity were calculated for KM ECG recordings, considering the individual leads and the combinations of 2-lead and the 3-lead. Analysis was accomplished for all STEMI cases and separately for anterior and inferior STEMI cases. Because the sensitivity and specificity are equally important in determining the validity of the smartphone ECG, Youden's J statistic was calculated as sensitivity plus specificity minus 1. The closer the value is to 1, the better the agreement between the smartphone ECG and the 12-lead ECG. The positive and negative predictive values are related with prevalence of the disease, but the proportion of STEMI/healthy cases in this study is far from being representative of the real prevalence, so those values are not provided.
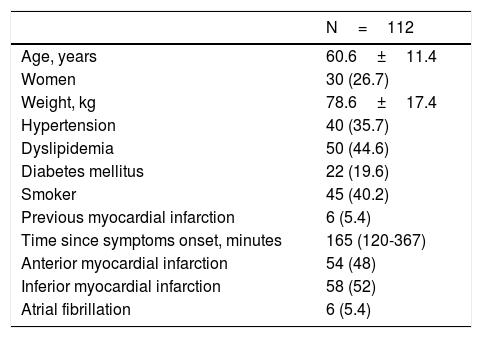
ResultsA total of 112 consecutive patients with diagnosis of STEMI were included, meeting all inclusion and exclusion criteria. The demographic and clinical characteristics are listed in Table 1.
Characteristics of patients included.
| N=112 | |
|---|---|
| Age, years | 60.6±11.4 |
| Women | 30 (26.7) |
| Weight, kg | 78.6±17.4 |
| Hypertension | 40 (35.7) |
| Dyslipidemia | 50 (44.6) |
| Diabetes mellitus | 22 (19.6) |
| Smoker | 45 (40.2) |
| Previous myocardial infarction | 6 (5.4) |
| Time since symptoms onset, minutes | 165 (120-367) |
| Anterior myocardial infarction | 54 (48) |
| Inferior myocardial infarction | 58 (52) |
| Atrial fibrillation | 6 (5.4) |
Data presented as n (%), mean±standard deviation or median (interquartile range).
KM ECG recordings were obtained in all cases. The rate of poor quality/unreadable recording was 8%, 1.7% and 3.5% for leads I, II, and anterior precordial respectively. Of note, among those recordings showing ST changes, these consisted mostly in depression in all leads (76%, 70%, and 78% respectively). Discrepancy between the 2 blinded investigators was very low (5.3%).
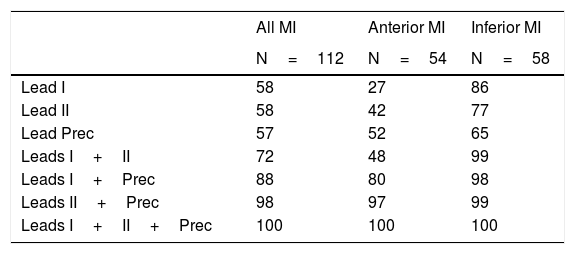
The values for sensitivity are shown in Table 2. Sensitivity was modest for individual leads (57-58%) though higher for inferior STEMI (65-86%) as compared to anterior STEMI (27-52%). The leads I and II yielded higher sensitivity in inferior STEMI and the precordial lead resulted more sensitive to anterior STEMI. The combination of 2 leads (particularly when including the precordial lead) and the combination of 3 leads markedly increased the sensitivity for both inferior and anterior STEMI.
Sensitivity of Kardia Mobile system for detection of ST changes.
| All MI | Anterior MI | Inferior MI | |
|---|---|---|---|
| N=112 | N=54 | N=58 | |
| Lead I | 58 | 27 | 86 |
| Lead II | 58 | 42 | 77 |
| Lead Prec | 57 | 52 | 65 |
| Leads I+II | 72 | 48 | 99 |
| Leads I+Prec | 88 | 80 | 98 |
| Leads II+Prec | 98 | 97 | 99 |
| Leads I+II+Prec | 100 | 100 | 100 |
Data presented as %.
MI, myocardial infarction; Prec, precordial.
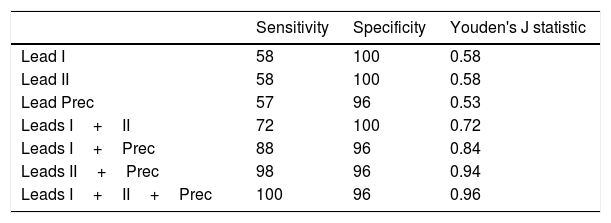
As indicated in methods, for the purpose of specificity analysis, KM ECG recordings were obtained from 25 healthy individuals showing strictly normal conventional 12-leads electrocardiography recordings. Table 3 presents the specificity and the Youden's J statistic along with the previously described sensitivity. Specificity was generally very high and the J statistic was excellent for the 2-lead combinations that included the precordial lead and for the 3-lead approach.
Sensitivity, Specificity and Youden's J statistic of Kardia Mobile system for detection of ST changes.
| Sensitivity | Specificity | Youden's J statistic | |
|---|---|---|---|
| Lead I | 58 | 100 | 0.58 |
| Lead II | 58 | 100 | 0.58 |
| Lead Prec | 57 | 96 | 0.53 |
| Leads I+II | 72 | 100 | 0.72 |
| Leads I+Prec | 88 | 96 | 0.84 |
| Leads II+Prec | 98 | 96 | 0.94 |
| Leads I+II+Prec | 100 | 96 | 0.96 |
Data presented as % (sensitivity and specificity) or ratio (Youden's J statistic).
Prec, precordial.
Several cases are shown in Fig. 1, Fig. 2, and Fig. 3 which are illustrative of the reported results.
The results of this study can be summarized as follows: a) KM recordings can easily be obtained in patients with STEMI with adequate quality in the vast majority of cases; b) ST changes consist mostly in depression; c) sensitivity for single leads is modest and differs according to infarction location but specificity seems to be high; and d) sensitivity for combination of leads improves markedly, specifically for the 2-lead including the precordial and for the 3-lead combination.
STEMI remains nowadays a serious health condition. Suffering STEMI has been drastically ameliorated by reperfusion therapies, especially by primary angioplasty. Nonetheless, to obtain the best clinical outcome STEMI patients require immediate reperfusion treatment. It has been reported that one third of patients with non-reperfused STEMI will die within the first 24hours of the event.15
The mortality of STEMI concentrates in the prehospital setting within the first 2hours, usually occurring from cardiac arrhythmias (ventricular fibrillation). On the other hand, and despite public health education programs it is common that many patients experiencing a STEMI do not seek medical care for up to 2hours after symptom onset.1–3 This patient-related delay accounts for many deaths occurring in the first 2hours after symptoms onset but also for a decreased rate of myocardial salvage derived from the late application of reperfusion therapies, mainly primary angioplasty. The reasons for such a delay in seeking medical attention have been well described and include such issues as lack of STEMI identification, misattributing symptoms of STEMI to some other disease, fearing embarrassment of false alarm, not fitting a “stereotype” for heart disease, and lack of recognition by bystanders of a STEMI event.16
The earlier treatment of STEMI reduces mortality and morbidity, so it becomes crucial to increase the speed of recognizing that a STEMI event is occurring. The ECG remains the essential method for diagnosing STEMI and it is also the simplest and most accessible diagnostic modality. Immediate access to an ECG recording just when symptoms appear could potentially accelerate the demand of medical care by the patient.
Smartphone technologies have become widespread and readily available in every country in the world. Several medical applications (apps) have been developed in recent years with the aim to improve point of care contacts and to increase patient access to timely care, including ECG apps.
The pocket-sized KardiaMobile involves the use of a pair of electrodes linked to a mobile device to provide a single-lead rhythm strip. With minimal training, 2 fingers from each hand are placed on the monitor (which can be connected to the back of a smartphone) for 30seconds to take an ECG recording, which is wirelessly transmitted to the app, analysed and synchronised to an encrypted server. The patient can then alert their healthcare professional to allow the ECG to be viewed securely. The device was initially developed for detecting atrial fibrillation. It uses a US Food and Drug Administration–cleared automatic algorithm with 98% sensitivity and 97% specificity reported for the diagnosis of atrial fibrillation.9
As a result of the success of single lead smartphone-based rhythm evaluation, ST segment and T wave changes during myocardial ischemia have been evaluated by using a “12-lead equivalent” approach through the use of the AliveCor Heart Monitor.11,12 This is a Food and Drug Administration -approved class II medical device, paired with a 5th generation iPod Touch device. The device used in these studies was a modified one with 2 electrical leads connected to wires with alligator clips, which are then attached to the same adhesive stickers used in the standard 12-lead ECG. This single lead system allowed to obtain a virtual 12 leads ECG in 204 subjects complaining of chest pain (57 with confirmed STEMI) yielding a sensitivity and specificity for STEMI of 89% and 84% respectively.12 Nonetheless, this system is deemed appropriate as a screening diagnostic tool to be used by healthcare/emergency staff at direct point of care.
The KardiaMobile system used in our study is a pocket sized device, designed to be used by the general population, by any layperson with access to a smartphone. To our knowledge, our study is the largest published so far addressing the detection of ST changes by a smartphone-based ECG system and the first using the KardiaMobile system. The study demonstrates that this user-friendly smartphone-based system when used to get a combination of 2 or 3 leads recordings may yield a high sensitivity and specificity in the detection of ST changes during STEMI.
The potential implications of these findings would be to validate the possibility of obtaining 2-3 leads ECG recording very easily using a portable sensor device linked to a smartphone application, used as a screening method for ST changes in the presence of chest pain.
This technology would be very accessible to people suspicious of symptoms or to paramedical professionals or other type of public agents that attend these persons in the first place. This represents a great advance in patient empowerment and in their engagement with the healthcare process. Nonetheless, there are important aspects to consider. The quality of the recordings should be as high as possible. The interpretation of the recordings should be done automatically through an algorithm that needs to show sensitivity as close to 100% as possible, even if this is somehow detrimental to the specificity. The development of such algorithms appears complex and challenging but no doubt it will be accomplished. The recording should be sent immediately to a health emergency service. All this requires very important technological, logistical and regulatory developments that take into account study result, implications on liability and the availability of health resources.
The most critical concern comes from the possibility that a patient who is actually suffering from STEMI, non-STEMI acute coronary syndromes (unstable angina or non-ST elevated myocardial infarction) or another serious condition associating similar symptoms (pulmonary embolism or aortic dissection) may refrain to demand medical care because of a false negative, a true negative or a poor quality recording.
For this reason, implementing these applications to the general population must be associated with an important effort on education and communication. Larger studies are warranted to confirm sensitivity and particularly specificity, considering a more precise estimate of the prevalence of STEMI, not over the general population, but rather over the population complaining of symptoms that are compatible with STEMI.
LimitationsThe application of KM by trained healthcare personnel could provide better recordings than those expected if applied by the general population. However, with adequate training, everybody could be able to get high quality recordings in the 3 leads.
Although a new version of this KM system has recently been released, the Kardia 6L, which allows to obtain more than 3 leads, the present study uses the much more widely used version, and also these results could be relatively applied to this newer system.
A higher number of patients both with and without STEMI could be required to ascertain more properly the sensitivity and particularly the specificity. Specificity could be lower in healthy patients showing ECG alterations such as early repolarization or right bundle branch block. Furthermore, these changes are also prevalent in several cardiac conditions other than STEMI.12 Nonetheless, the KM, like other similar systems, is designed to serve as a screening diagnostic methods, thus it must specifically show a very high sensitivity and a relatively, but not necessarily, high specificity.
Reliable positive and negative predictive values could not be provided since these parameters are strongly related with the prevalence of the condition, but the proportion of STEMI/healthy cases in this study is far from being representative of the real prevalence of STEMI among those presenting more or less compatible symptoms.
Finally, the interpretation of the recordings should be done automatically through an algorithm with what appears to be quite a complex and challenging development.
ConclusionsThe Kardia Mobile system using 2-lead combination (particularly I plus precordial or II plus precordial) or 3-lead shows a very high sensitivity for both anterior and inferior STEMI. Larger studies are warranted including population complaining of symptoms compatible with STEMI with or without subsequent confirmation.
There are several systems based on smartphone applications that can be used to obtain electrocardiographic recordings.
The KardiaMobile has been validated for the detection of arrhythmias, but its diagnostic value in detecting ST changes in patients suffering from an ST elevated myocardial infarction is unknown.
Does it contribute anything new?This is the largest study carried out to evaluate the diagnostic sensitivity of the KardiaMobile system for detecting ST changes in patients with ST elevated myocardial infarction.
The KardiaMobile showed a modest sensitivity using isolated leads but a very high sensitivity with the combination of 2 or 3 leads, always including the anterior precordial one.
No funding required for this study.
Conflicts of interestThe authors declare no conflict of interest in this article.